One study showed that men, black people, and older patients were more likely to catch COVID, while those taking melatonin, paroxetine, or carvedilol were less likely to do so.
In diseases with a high degree of inflammation, melatonin use is very promising, as it lowers circulating cytokine levels. Melatonin has also been shown to be beneficial in patients who have suffered a heart attack, or those with cardiomyopathy, hypertensive heart disease, and pulmonary hypertension.
Dr. Alfonso Galán González – Neolife Medical Team
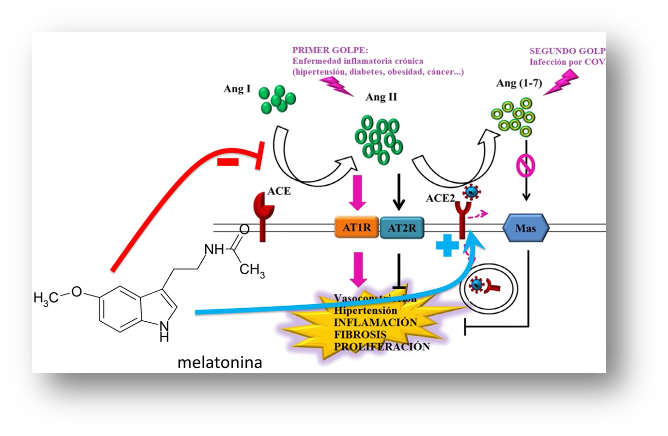
SThere is a hypothesis that has been proposed that the RAS suffers two blows that lead to the progression of COVID-19 disease in patients with a history of inflammation.
The first would come from the low-grade inflammation associated with diseases that cause chronic inflammation, and the second blow is caused by COVID. This may explain the higher mortality rate in patients with this type of pathology.
In these blog posts, we have often referred to this incredible molecule (here), and we’ve even mentioned how beneficial it is in coronavirus disease (here).
This time, we will delve deeper (even at the molecular level) into what makes melatonin have these effects, presenting the research that supports these findings.
What are the effects of melatonin that may help us combat COVID-19?
They are summarized in this chart:

In this first part, we will talk about its antiviral, anti-inflammatory, antioxidant, chronobiotic, and immunomodulatory effects, leaving the rest, together with an explanation of the studies currently underway, for a second blog post.
ANTIVIRAL EFFECT
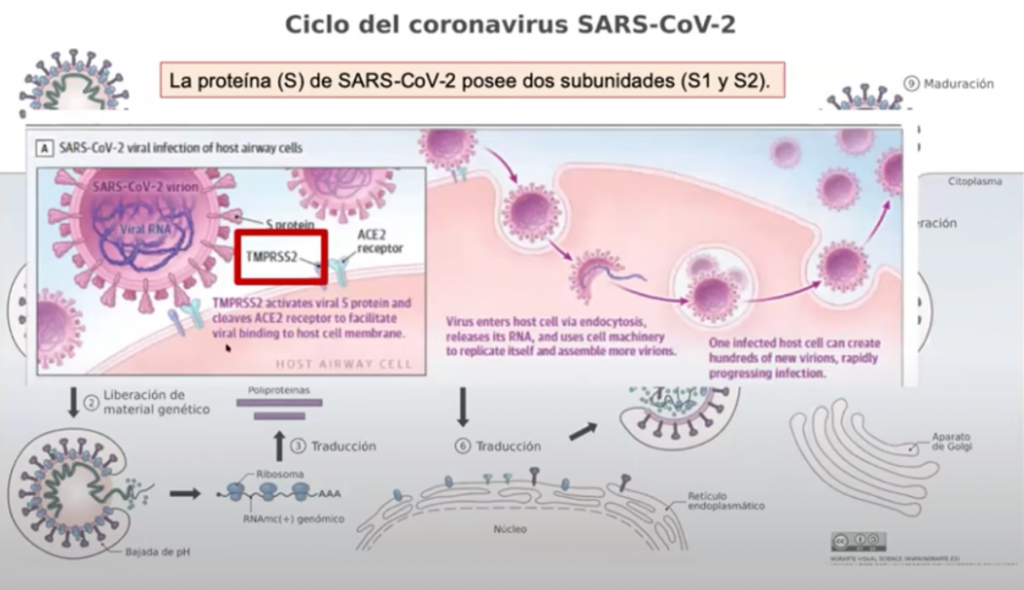
SARS-CoV-2 enters the pulmonary epithelial cells and others through the ACE2 receptor.
The glycoprotein spike on the surface of the virus is bound to the ACE2 receptor (angiotensin-converting enzyme 2); after membrane fusion, the viral RNA genome is released into the cytoplasm and results in two polyproteins that are split by the SARS-CoV-2 main protease, which results in the replication-transcription complex.
Melatonin has been shown to inhibit the virus protease more effectively than other ligands.
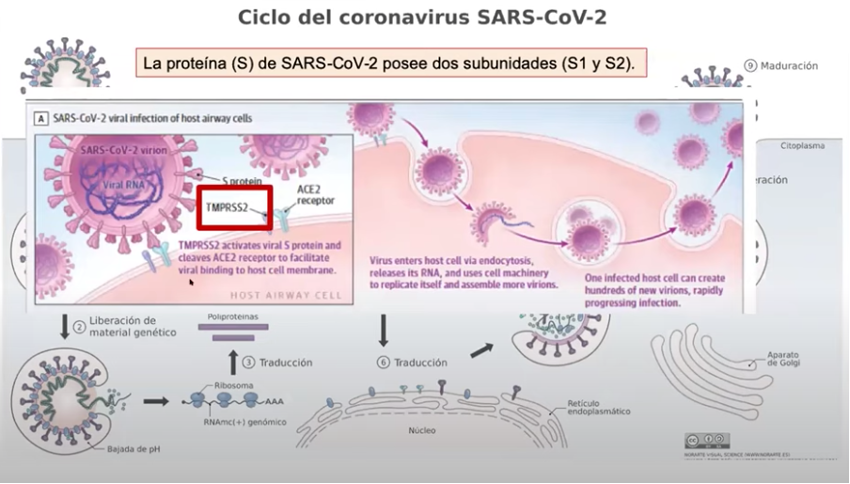
Another way in which it may regulate infection is by binding and inhibiting calmodulin, which regulates the expression and retention of ACE2 in the cell membrane.
One study showed that men, black people, and older patients were more likely to catch COVID, while those taking melatonin, paroxetine, or carvedilol were less likely to do so.
The relationship between COVID and melatonin and the Renin-Angiotensin System (RAS) goes somewhat further. In general, RAS induces inflammation, high blood pressure, vasoconstriction, fibrosis, and proliferation via the ACE2/angiotensin II/AT1R axis and the opposite effects via the ACE2/angiotensin (1-7)/MAS axis.
The RAS is activated by chronic inflammation in cancer, diabetes, high blood pressure, and obesity. SARS-CoV-2 induces the internalization and detachment of ACE2, which leads to the inactivation of the ACE2 / angiotensin (1-7) / MAS axis.
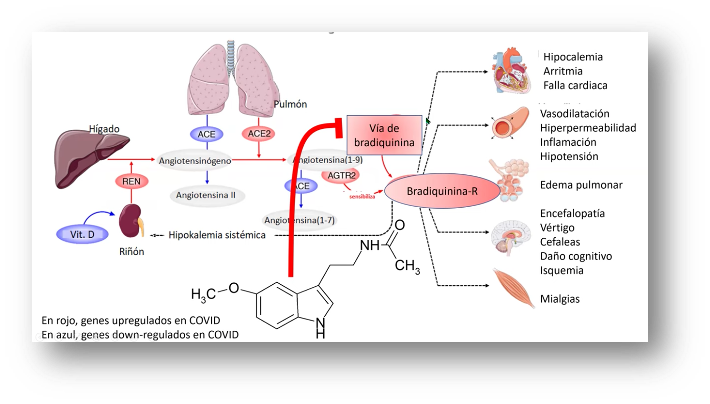 And so, there is a hypothesis that has been proposed that the RAS suffers two blows that lead to the progression of COVID-19 disease in patients with a history of inflammation. The first would come from the low-grade inflammation associated with these diseases that activate the ACE/angiotensin II/AT1R axis, and the second blow is triggered by COVID, as it renders the ACE2/angiotensin (1-7)/MAS axis inactive. This may explain the higher mortality rate in patients with this type of pathology.
And so, there is a hypothesis that has been proposed that the RAS suffers two blows that lead to the progression of COVID-19 disease in patients with a history of inflammation. The first would come from the low-grade inflammation associated with these diseases that activate the ACE/angiotensin II/AT1R axis, and the second blow is triggered by COVID, as it renders the ACE2/angiotensin (1-7)/MAS axis inactive. This may explain the higher mortality rate in patients with this type of pathology.
Melatonin is an effective angiotensin II activation inhibitor and facilitates the action of angiotensin (1-7), thus acting on both “blows”.
Anti-inflammatory/Immunoregulatory Effect
Immunoregulation
T cells are the most advanced cells in our immune system. For a somewhat more complete explanation of how our immune system works, please read this blog post.
For the purposes of this blog post, we will mention a few types of white blood cells (a fundamental cell of the adaptive immune system). There are T helper cells (Th cells), also known as CD4+ cells, that include Th1, Th2, Th17, and T regulators (Treg) (CD4+ CD 25+).
Despite the complexity of the immune system, the fundamentals of its functioning are based on 3 white blood cell populations, the Th1, the Treg, and the Th17. Th cells activate Treg, inhibit Th17, and promote antigen-independent cytotoxicity by inducing the evolution of NK (Natural Killer) cells from our innate immune system into natural killer cells that are activated by lymphokines. Their actions are usually mediated by the secretion of IL-2, the main growth factor for white blood cells.
The relationships between these subtypes of white blood cells are markers for the main diseases suffered by human beings. And so:
- A low ratio of Th1 to Treg is typical in advanced neoplasia.
- A higher ratio of Th17 to Treg is typical in autoimmune diseases… and acute respiratory distress induced by coronavirus.
Anti-inflammatory
The main pathophysiological mechanism of SARS-CoV-2 infection is upward regulation of pro-inflammatory cytokines induced by the activation of neutrophils, macrophages, and mast cells. They increase IL-1, IL-6, and IL-17, C-reactive protein, and TNF alpha.
Melatonin exerts its anti-inflammatory effects through various mechanisms:
- One of these is the Sirtuin 1 mechanism, which prevents macrophages from becoming the pro-inflammatory type.
- It suppresses NF-kB activity.
- It stimulates the production of Nrf2 in studies of heart and liver protection.
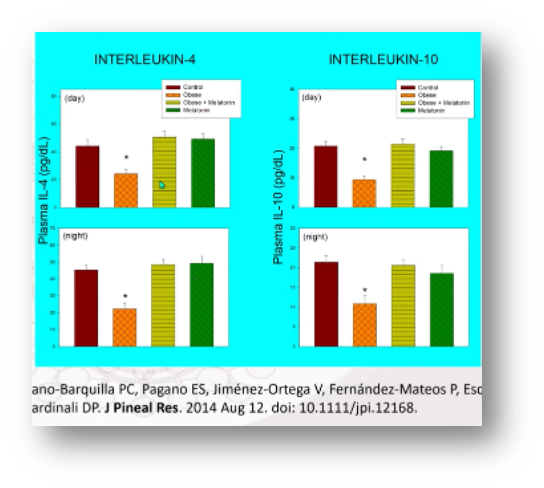
- It reduces pro-inflammatory CK (TNF-alpha, IL-1, IL-6, IL-8, and IL-17) and increases anti-inflammatory ones such as IL-10.
Even though all these terms are too scientific, the charts helps us understand them, and it’s interesting to see the mechanism through which they exert their effects.
.
And so, the charts below show how doses of 60 mg of melatonin inhibit the production of pro-inflammatory cytokines.
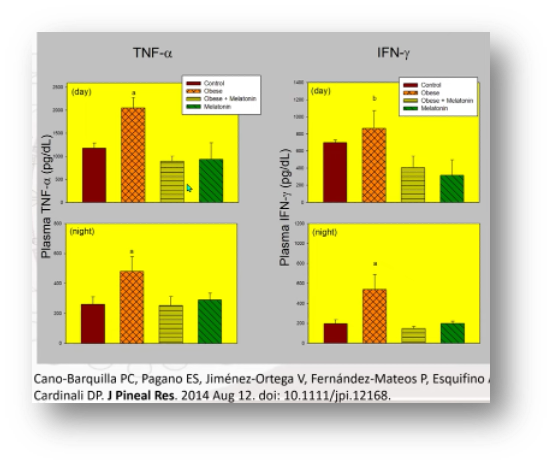
And increases the anti-inflammatory kind.
 Coronavirus infection accumulates hyper-inflammatory monocytes and macrophages in the lower respiratory tract, where they play a key role in determining whether the disease will be severe. Infected monocytes and macrophages change their metabolism from oxidative phosphorylation in the mitochondria to glycolysis in the cytoplasm, generating reactive oxygen species; these monocytes that obtain their energy in this way produce more cytokines, causing the destruction of T cells and alveolar cells, thus aggravating the infection.
Coronavirus infection accumulates hyper-inflammatory monocytes and macrophages in the lower respiratory tract, where they play a key role in determining whether the disease will be severe. Infected monocytes and macrophages change their metabolism from oxidative phosphorylation in the mitochondria to glycolysis in the cytoplasm, generating reactive oxygen species; these monocytes that obtain their energy in this way produce more cytokines, causing the destruction of T cells and alveolar cells, thus aggravating the infection.
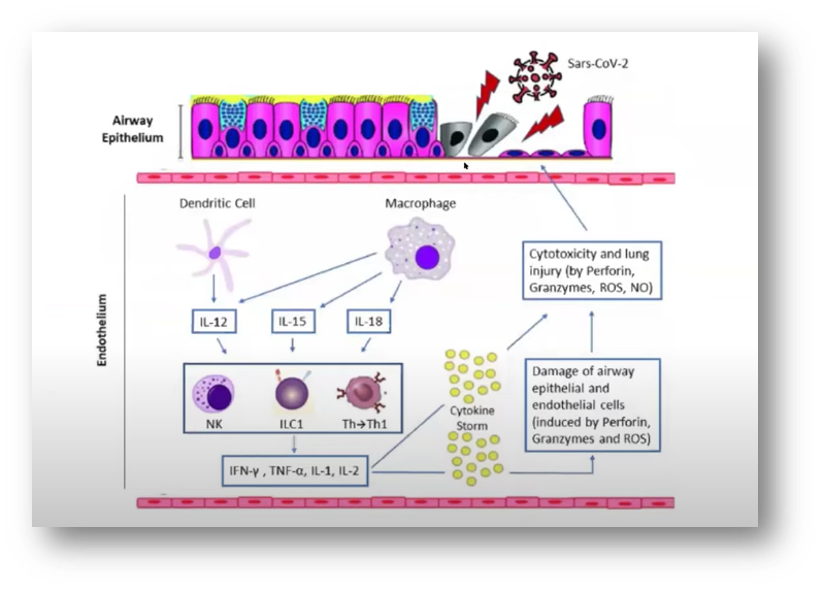
Melatonin converts these macrophages with modified metabolism back into M2 anti-inflammatory macrophages that use oxidative phosphorylation.
Antioxidant Effect
In both the cytoplasm and nucleus, melatonin has important antioxidant effects and purifies free radicals. These effects are achieved in 3 ways:
- Melatonin eliminates free radicals.
- Melatonin is metabolized into compounds with great antioxidant power.
- It is a direct antioxidant that stimulates the synthesis of antioxidant enzymes and inhibits pro-oxidants.
- It enhances the effects of other antioxidants such as Vitamin C.
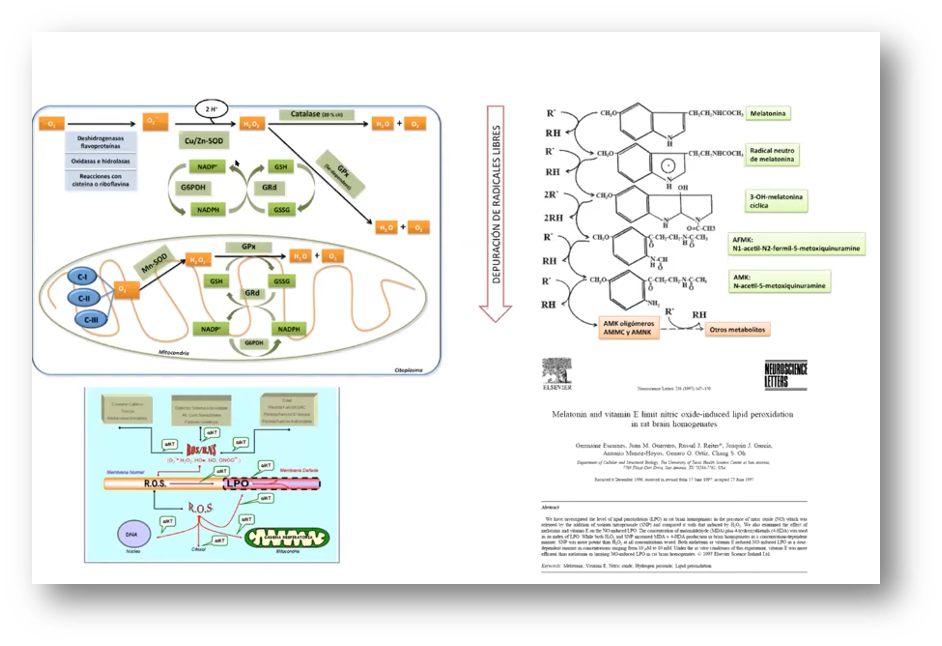
As shown in this graphic, there is an intimate relationship, a kind of “vicious circle”, between the production of Reactive Oxygen Species (ROS) and free radicals and inflammation.
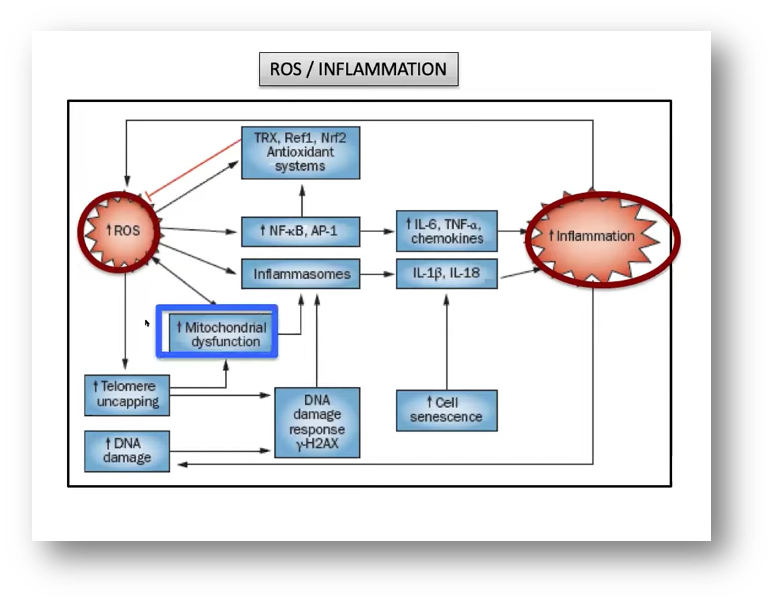
One feeds the other and vice versa. In diseases with a high degree of inflammation, melatonin use is very promising, as it lowers circulating cytokine levels. This has been documented in patients with DM2, periodontal disease, and severe multiple sclerosis, as well as in acute inflammation, such as surgical stress, cerebral or coronary reperfusion.
Generally speaking, these effects are achieved with doses that are higher than those used for a chronobiotic effect (2-3 times, of about 100-300 mg).
SEPSIS
Clinical data for COVID-19 disease show us that these patients are at higher risk of sepsis and heart failure.
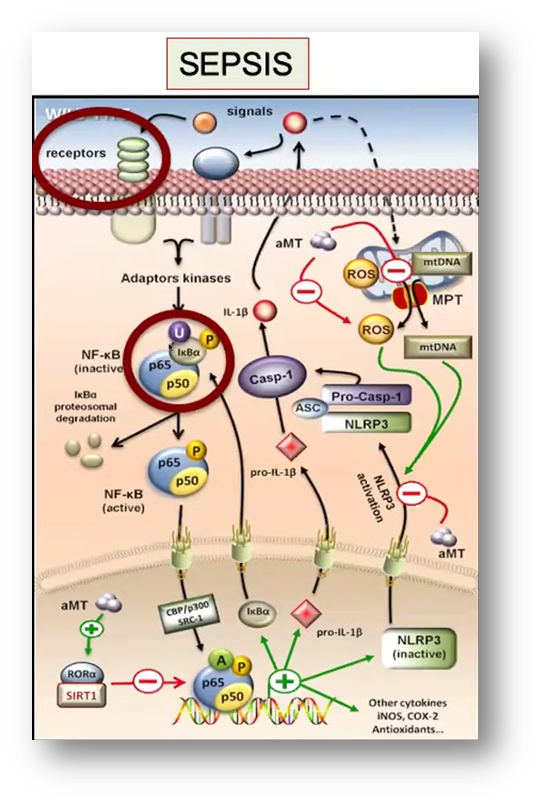
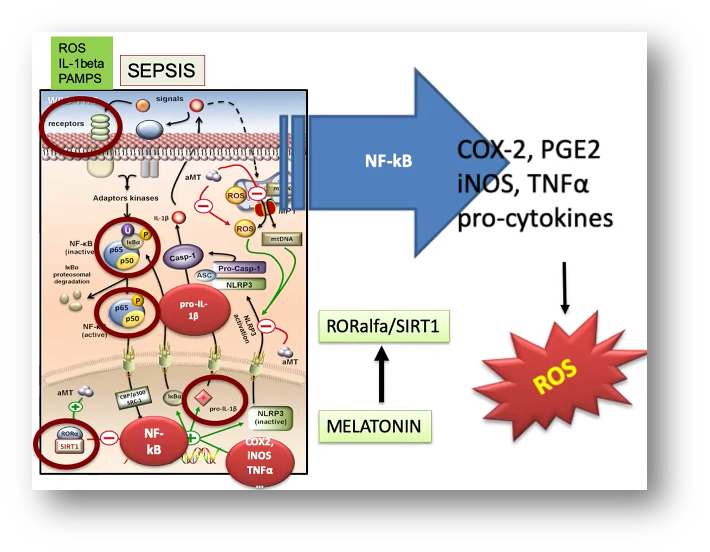
Melatonin improves the septic shock by inhibiting the NLRP3 pathway, called inflammasome. What is this? The inflammasome is a complex that promotes the maturation of pro-inflammatory cytokines such as IL-1o and IL-18. The inflammasome is responsible for the activation of inflammatory processes, and there is evidence that shows it induces cellular pyroptosis, a highly inflammatory form of scheduled lytic cell death that occurs most often after infection with intracellular pathogens.
Melatonin has been shown, in rodents, to improve kidney, myocardial and liver damage in cases of sepsis, and in human neonatal sepsis, it improves clinical evolution.
In the study represented in these graphs, it was shown to increase the average lifespan of mice with peritonitis.
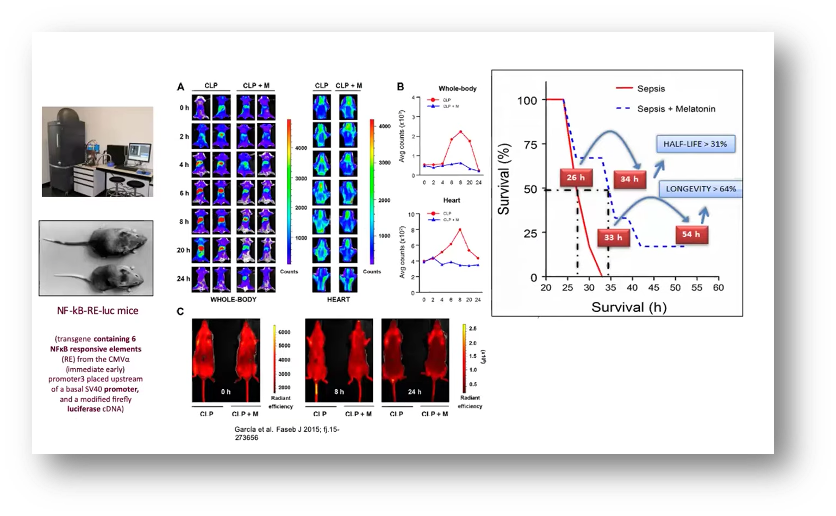
Melatonin has also been shown to be beneficial in patients who have suffered a heart attack, or those with cardiomyopathy, hypertensive heart disease, and pulmonary hypertension.
In critical patients, even those admitted to ICU, deep sedation increases long-term mortality. The use of melatonin in these patients lowers the use of sedation, pain, agitation, anxiety, and improves sleep quality.
A study of 10 patients admitted to the hospital with COVID-related pneumonia and poor prognostic risk factors administered melatonin, between 36 and 73 mg daily, along with standard treatment. Benefits were observed in all clinical variables (symptoms, regression of pulmonary infiltrates, inflammation markers), as well as in the need for ventilation, total hospitalization time, and final result (death vs recovery).
Another current article in the “preprint” phase shows data from 791 patients who required intubation from severe COVID lung disease and retrospectively analyses which treatments improved prognosis. Melatonin was the only treatment significantly associated with a better evolution.
Chronobiotic Effect
This refers to molecules that affect the physiological regulation of the body clock and specifically those capable of recovering unsynchronized circadian rhythms or preventing this from happening.
The elderly population is not only more susceptible to coronavirus infection but is more likely to have circadian rhythms that are altered by several causes, such as melatonin levels that decrease with age or an increase in stress from social isolation. The deregulation of circadian rhythms is believed to be involved in multiple pathologies suffered in the elderly, especially cardiovascular and neurodegenerative diseases.
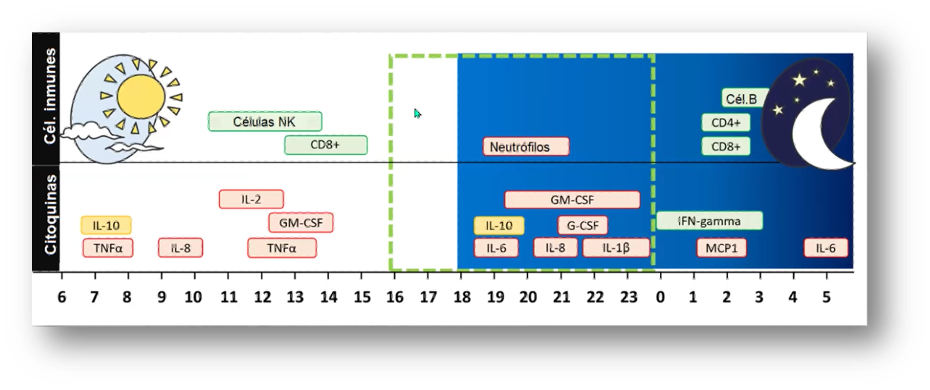
It is worth noting that our immune system shows a significant circadian rhythmicity. Therefore, at the start of the day’s activity, there is greater expression of pro-inflammatory CK such as IL-1, IL-6 and IL-12 as well as macrophagic and leukocyte activity that leads to possible tissue damage. By contrast, anti-inflammatory mediators and other growth and angiogenesis factors are increased in the resting phase. As for immune cells; CD4 and CD8 activity against viral antigens reach their maximum levels in the resting phase, while cytotoxic activity of NK cells is more severe in the early hours of activity.
Indeed, these patterns may be altered in older people and should be taken into account when administering immunomodulators or anti-inflammatory drugs.
Delirium
Cases of delirium are found in 50% of hospitalized older patients and 80% of those in critical condition who require mechanical ventilation. Melatonin use is associated with lower ICU stay, lower prevalence of delirium, and improved sleep quality.
In COVID-19 disease, 15% of hospitalized patients have some degree of impaired of consciousness, from drowsiness to coma. Melatonin should be considered an effective agent for improving sleep and minimizing administration of BZD and antipsychotics.
With this, we end this first part of how melatonin may improve COVID disease. I hope it wasn’t too complicated to understand. I recommend you stay tuned for Part 2, which is very interesting, as well, and which provides insights into how its use is being integrated into the different fields and medical specialties.

BIBLIOGRAFÍA
(1) Gurwitz, D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Dev. Res. 2020, 81, 537–540.
(2) Hardeland, R. Melatonin and inflammation—Story of a double-edged blade. J. Pineal Res. 2018, 65, e12525.
(3) Xia, Y.; Chen, S.; Zeng, S.; Zhao, Y.; Zhu, C.; Deng, B.; Zhu, G.; Yin, Y.; Wang, W.; Hardeland, R.; et al. Melatonin in macrophage biology: Current understanding and future perspectives. J. Pineal Res. 2019, 66, e12547.
(4) Sánchez-López, A.L.; Ortiz, G.G.; Pacheco-Moises, F.P.; Mireles-Ramírez, M.A.; Bitzer-Quintero, O.K.; Delgado-Lara, D.L.C.; Ramírez-Jirano, L.J.; Velázquez-Brizuela, I.E. Efficacy of Melatonin on Serum Pro-inflammatory Cytokines and Oxidative Stress Markers in Relapsing Remitting Multiple Sclerosis. Arch. Med. Res. 2018, 49, 391–398
(5) Gitto, E.; Reiter, R.J.; Amodio, A.; Romeo, C.; Cuzzocrea, E.; Sabatino, G.; Buonocore, G.; Cordaro, V.; Trimarchi, G.; Barberi, I. Early indicators of chronic lung disease in preterm infants with respiratory distress syndrome and their inhibition by melatonin. J. Pineal Res. 2004, 36, 250–255.
(6) Gitto, E.; Karbownik, M.; Reiter, R.J.; Xian Tan, D.; Cuzzocrea, S.; Chiurazzi, P.; Cordaro, S.; Corona, G.; Trimarchi, G.; Barberi, I. Effects of melatonin treatment in septic newborns. Pediatr. Res. 2001, 50, 756–760.
(7) Castillo, R.R.; Quizon, G.R.A.; Juco, M.J.M.; Roman, A.D.E.; De Leon, D.G.; Punzalan, F.E.R.; Guingon, R.B.L.; Morales, D.D.; Tan, D.-X.; Reiter, R.J. Melatonin as adjuvant treatment for coronavirus disease 2019 pneumonia patients requiring hospitalization (MAC-19 PRO): A case series. Melatonin Res. 2020, 3, 297–310
(8) Ramlall, V.; Zucker, J.; Tatonetti, N. Melatonin is significantly associated with survival of intubated COVID-19 patients. medRxiv 2020
(9) Chellappa, S.L.; Vujovic, N.; Williams, J.S.; Scheer, F.A.J.L. Impact of Circadian Disruption on Cardiovascular Function and Disease. Trends Endocrinol. Metab. 2019, 30, 767–779.
(10) Zambrelli, E.; Canevini, M.; Gambini, O.; D’Agostino, A. Delirium and sleep disturbances in COVID–19: A possible role for melatonin in hospitalized patients? Sleep Med. 2020, 70, 111.