Progesterone is produced in the corpus luteum of the ovaries, a temporary gland that is developed once the egg is released from the ovary after it has matured. The Replenish study showed an improvement in the quality of life of patients who received this therapy.
Studies show that progesterone is able to reduce hot flashes associated with menopause even in the absence of treatment with estradiol. It is converted into allopregnanolone in the brain, which produces effects on the GABAergic system and induces sleep. Also, when used in conjunction with estradiol, it improves bone mineral density (BMD), among many other benefits.
Dr. Alfonso Galán González – Neolife Medical Team
Is it merely the inevitable companion of estradiol in Hormonal Replacement Therapy for menopause?
Progesterone is produced in the corpus luteum of the ovaries. It’s a temporary gland that is developed once the egg is released from the ovary after it has matured.
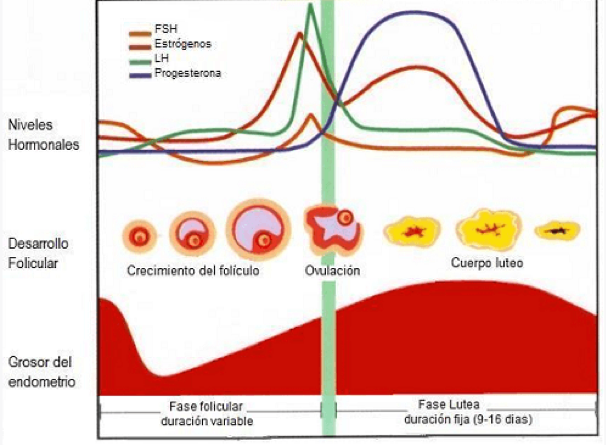
The adrenal glands and the uterus may also produce some progesterone. Progesterone helps prepare the body for pregnancy and causes the endometrium to thicken to receive the fertilized egg. If fertilization does not occur, the corpus luteum is destroyed causing a sharp decrease in this hormone, which in turn causes the endometrium to detach, leading to the onset of menstruation. If the egg is fertilized, the corpus luteum is not destroyed and continues to produce progesterone which, among other things, increases the blood supply to the endometrium, which allows nutrients to reach the embryo that is being formed. When the placenta forms, it also produces progesterone. Levels remain high throughout pregnancy.
Use in HRT (Hormone Replacement Therapy)
The known use of progesterone in this type of treatment is to prevent the proliferation of the endometrium and endometrial cancer when we use estradiol to replenish hormonal levels during menopause and to reverse the harmful effects that accompany the climateric, which are widely known (1).
At this point, we’ll consider a number of things related to the additional effects of providing bioidentical progesterone in HRT and the advantages it has over treatments with progestins (synthetic derivatives of non-bioidentical progesterone).
- There are studies that show that it is able to reduce hot flashes associated with menopause even in the absence of treatment with estradiol.
- The REPLENISH study showed an improvement in the quality of life of patients who received this therapy.
- Progesterone is converted into allopregnanolone in the brain, which produces effects on the GABAergic system and induces sleep.
- When used in conjunction with estradiol, it improves bone mineral density (BMD).
- A systematic review of the literature and analysis of studies conducted on women using estradiol with or without progesterone showed that there was no association between taking estradiol alone and the risk of breast cancer; however, the risk was higher when estradiol was combined with synthetic derivatives such as MPA (medroxyprogesterone), norethisterone acetate or levonorgestrel, but not with bioidentical progesterone (2).
- The use of progesterone is not associated with the risk of venous thromboembolism in postmenopausal women. Several studies confirm this and show that the addition of synthetic derivatives of norpregnane are indeed associated with significant risk (3).
- The ELITE study tested the hypothesis of “hormonal timing”, that is, that an early initiation of HRT, rather than a late one, prevents the progression of atherosclerosis. According to their results, women with less than 10 years of menopause who received oral progesterone did not present a progression of the carotid intima-media thickness and these effects did not vary with the addition of progesterone (4). Progesterone also seems to be beneficial in women with myocardial ischemia. A study conducted on women with ischemic heart disease showed that it prolonged the onset of pain and that this time was prolonged by adding progesterone but not synthetic derivatives (medroxyprogesterone) (5).
- It is a well-known fact that oral estradiol increases HDL cholesterol (good cholesterol), decreases LDL (bad cholesterol), and increases triglycerides. These effects don’t seem to occur with the use of transdermal estradiol. The addition of progesterone increases or has no effect on these elements of the lipid profile.
- At the cognitive level, the addition of progesterone to the treatment with estradiol has a neutral effect on the cognitive changes a woman may experience.
In addition to these effects mentioned above, when used in the context of Hormonal Replacement Therapy (HRT) in menopause, progesterone is very beneficial in premenopausal women as it combats PMS symptoms, and decreases swelling and headaches associated with the menstrual period (6).
In terms of sexual arousal, a study shows that progesterone increases the activity of nitric oxide synthases, thus increasing vaginal relaxation and vascular blood flow in sexual arousal. Its effect on the GABAergic system would also intervene in sexual motivation.
At Neolife, we understand the various beneficial effects of this hormone, all of which we have tried to present in this article. We are proud to help many women by including it in their treatments.
BIBLIOGRAPHY
(1) Mirkin S. Evidence on the use of progesterone in menopausal hormone therapy. Climacteric. 2018 Aug;21(4):346-354.
(2) Cordina-Duverger E, Truong T, Anger A, et al. Risk of breast cancer by type of menopausal hormone therapy: a case-control study among post-menopausal women in France. PLoS One 2013;8: e78016
(3) Canonico M, Fournier A, Carcaillon L, et al. Postmenopausal hor- mone therapy and risk of idiopathic venous thromboembolism: results from the E3N cohort study. Arterioscler Thromb Vasc Biol 2010;30:340–5
(4) Hodis HN, Mack WJ, Henderson VW, et al. Vascular effects of early 48. versus late postmenopausal treatment with estradiol. N Engl J Med 2016;374:1221–31
(5) Rosano GM, Webb CM, Chierchia S, et al. Natural progester- one, but not medroxyprogesterone acetate, enhances the beneficial effect of estrogen on exercise-induced myocardial ischemia in postmenopausal women. J Am Coll Cardiol 2000;36:215–19
(6) Wyatt K, Dimmock P, Jones P, Obhrai M, O’Brien S. Efficacy of progesterone and progestogens in management of premenstrual syndrome: systematic review. BMJ 2001;323(7316):776‐80.
