A recently published study has strengthened the predictive value in disease and death where the waist/hip ratio (WHR) is greater than the BMI.
The study concluded that even if we have a normal weight according to the body mass index (BMI), if the waist/hip ratio is high then the risk of dying from cardiovascular disease increases by 87% in men and 48% in women.
A person with a normal BMI and a high WHR doubles their risk when compared to a person with an elevated BMI and normal WHR.
Tania Mesa – Nutritionist and Nurse from Neolife
The important consideration is not your BMI, but the amount and location of the body fat.
At Neolife we have a wealth of experience in carrying out anthropometry and body composition assessments. For this reason we have understood for a long time that the body mass index (BMI) is a value that is only indicative of a person’s weight by reference to their height: the index does not take into account what component is contributing to the weight, if the weight is fat, water, muscle etc. Typically a high BMI score is indicative of fatty tissue, but on occasion, although rarely the case, the weight is due to an excess of lean mass or fat-free mass (muscle, water etc.). You only have to see the BMI of professional athletes to understand that some of them could be classified as obese, when their percentage of fat is in reality normal. Their muscle mass is the main component of their weight and, as a result, they have no greater risk of developing any of the diseases normally associated with overweight or obesity.
For more than 40 years, medical institutions and scientific societies have classified an individuals weight according to their BMI, when it should really be based on the body fat percentage. And if we were more strict in our approach, the location of the body fat; specifically whether or not the fat is located in the intra-abdominal area, that is to say, around the abdominal viscera.
Classification of weight according to BMI*
Some medical authorities classify overweight and obesity by reference to the individuals fat percentage in accordance with the following criteria:
- Men
- Overweight where the fat percentage is between 21 and 25%
- Obesity where the fat percentage is above 25%
- Women
- Overweight where the fat percentage is between 31 and 33%
- Obesity where the fat percentage is above 33%
However, there is no general criterion for the classification of overweight and obesity according to the fat percentage or even how best to measure the same (plicometry, impedantiometry, DXA etc).
A new study (a different study) published in the Annals of Internal Medicine (1) further reinforces the predictive value in disease and death where the waist/hip ratio (WHR) is greater than the BMI. The authors found that a high WHR with a normal BMI is likely to cause an increase in the risk of disease and early death, particularly in relation to cardiovascular causes. The accumulation of intra-abdominal fat or visceral fat is a genuine risk factor. Fat that accumulates in the abdomen is not the same as fat on the legs or hips.

The study analyzed data from the NHANES III health survey (Third National Health and Nutrition Examination Survey) conducted on 15,184 people (52.3% women) between the ages of 18 and 90 over a period of more than 14 years. The study concluded that even if we have a normal weight according to the body mass index (BMI), if the waist/hip ratio is high then the risk of dying from cardiovascular disease increases by 87% in men and 48% in women. A person with a normal BMI and a high WHR doubles their risk when compared to a person with an elevated BMI and normal WHR.
In the editorial article in the same journal (2), Dr. Poirier discusses the usefulness of different techniques as a means to quantify abdominal obesity and recognizes that, although BMI is not the ideal technique when BMI is used together with waist circumference and/or the hip-waist ratio that it is the most appropriate technique in a clinical setting.
The simplest way to measure an accumulation of intra-abdominal fat is with a tape measure. You can simply measure the waist circumference to discover whether or not the individual concerned has a value greater than 80 cm (for women) and 94 cm (for men) that would be considered high (according to the IDF criteria, International Diabetes Federation). However, the WHO criteria is more relaxed: stating greater than 88 cm for women and 102 cm for men. Another way to assess intra-abdominal fat is to calculate the ratio between waist circumference and hip circumference and compare the ratio to the WHO criteria which states that a waist/hip ratio is high if the value is greater than or equal to 0.85 in women and 0.9 in men.
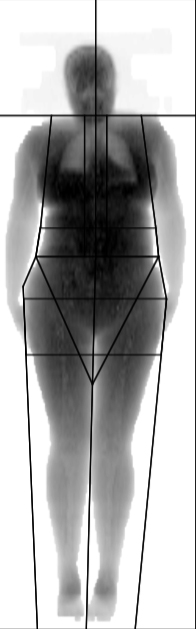
The ideal quantification technique to use for intra-abdominal fat remains the CAT scan (computerized axial tomography) and MRI (magnetic resonance imaging) but they are not useful in day-to-day clinical practice due to their cost, duration and radiation (in the case of a CAT scan). The intermediate alternative is DXA (dual-energy x-ray absorptiometry), which is the most sophisticated means of measuring body composition in a clinical setting. However, although this allows us to quantify fat in a certain region of the abdomen this method does not allow us to distinguish between visceral fat and subcutaneous fat within the defined area. And one must also note that there are no reference values.
At Neolife we perform a complete anthropometric assessment, which includes the following:
- BMI Calculation
- Determination of the waist circumference (WHR)
- Anthropometry using measurements from 6 fat folds, perimeters and diameters
- Multifrequency octopolar bioimpedantiometry
- DXA
- Morphological image assessment (technical photographs)
By combining all of these methods we have the best available clinical approach to anthropometric assessment as the results inform us in a very exact way about the risk(s) that excess weight can have on our health.
At Neolife we have extensive experience in carrying out body assessments
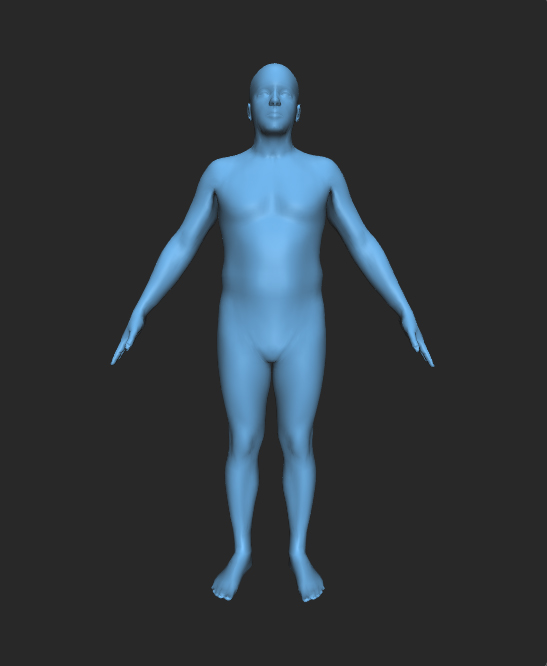
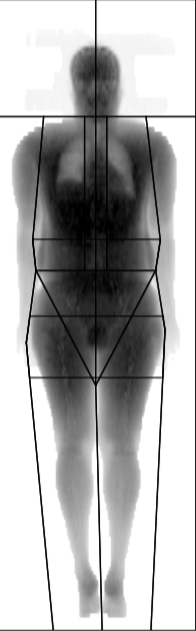
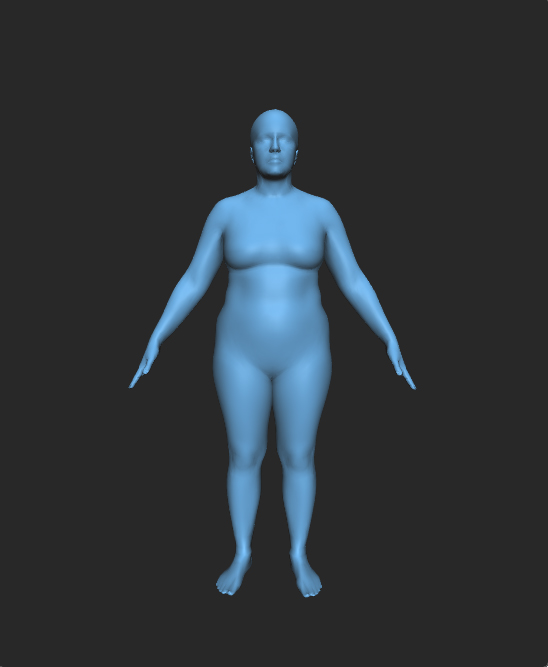
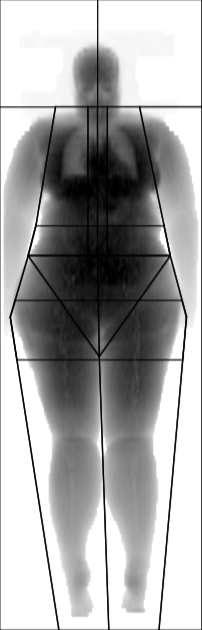
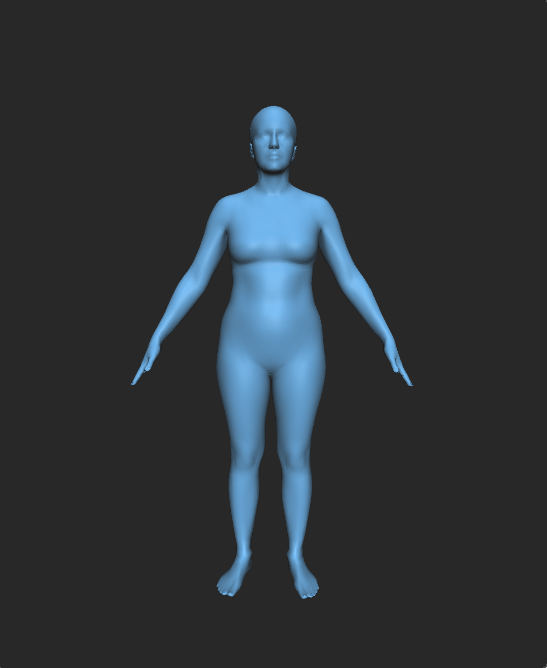
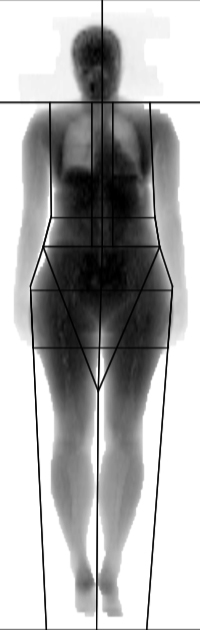
Below we have provided a few real-life cases from Neolife patients using a profile simulator based on their BMI and the image obtained of them through DXA:
Patient nº1 (man)
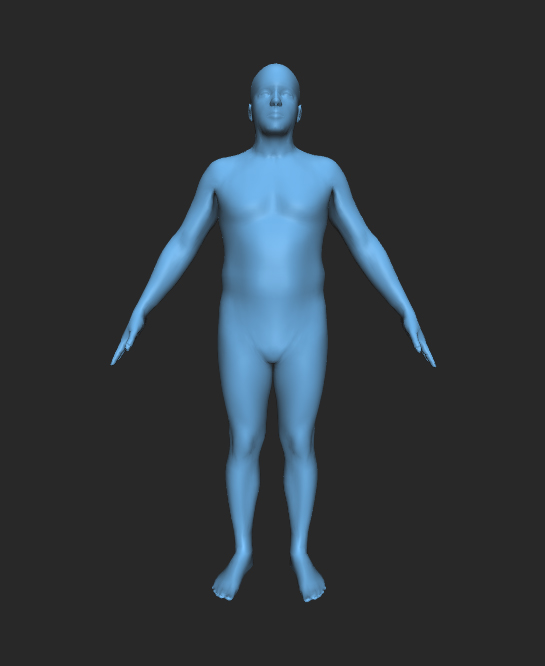
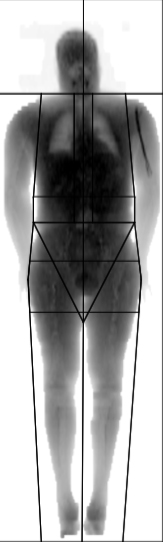
- BMI: 30.5 (obesity I)
- Waist: 95.4 (normal according to WHO)
- WHR: 95.4/106.5 = 0.89 (normal according to WHO)
- Total fat % from DXA: 22.1 (overweight)
- Abdominal region fat % from DXA: 27.9%
- Example of a high BMI with a not significantly high fat percentage, a normal waist circumference, a normal WHR and normal abdominal region fat percentage.
- OBESE ACCORDING TO BMI, INTRA-ABDOMINAL FAT NOT ELEVATED, CARDIOVASCULAR RISK NOT ELEVATED
Patient nº2 (man)
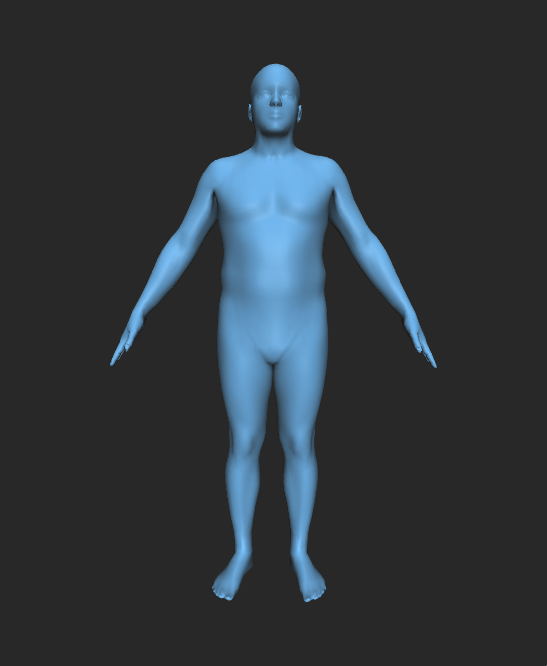
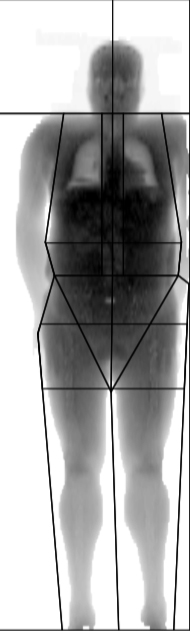
- BMI: 31.9 (obesity I)
- Waist: 112 (elevated according to WHO)
- WHR: 1.01 (elevated according to WHO)
- Fat % from DXA: 31.5 (obesity)
- Abdominal region fat % from DXA: 43.3%
- Example of a high BMI with a high fat percentage, elevated waist circumference, elevated WHR and high abdominal region fat percentage.
- OBESE ACCORDING TO BMI, INTRA-ABDOMINAL FAT ELEVATED ACCORDING TO DXA AND WHR, ELEVATED CARDIOVASCULAR RISK
Patient nº3 (male)
- BMI: 29.1 (grade 2 overweight)
- Waist: 93 (normal according to WHO)
- WHR: 0.9 (upper limit according to WHO)
- Fat % from DXA: 34.5 (obesity)
- Abdominal region fat % from DXA: 43.4%
- Example of a non-obese BMI with a high fat percentage, elevated waist circumference, elevated WHR and abdominal region fat percentage.
- NOT OBESE ACCORDING TO BMI, INTRA-ABDOMINAL FAT ELEVATED ACCORDING TO DXA AND WHR, ELEVATED CARDIOVASCULAR RISK
Patient nº4 (woman)
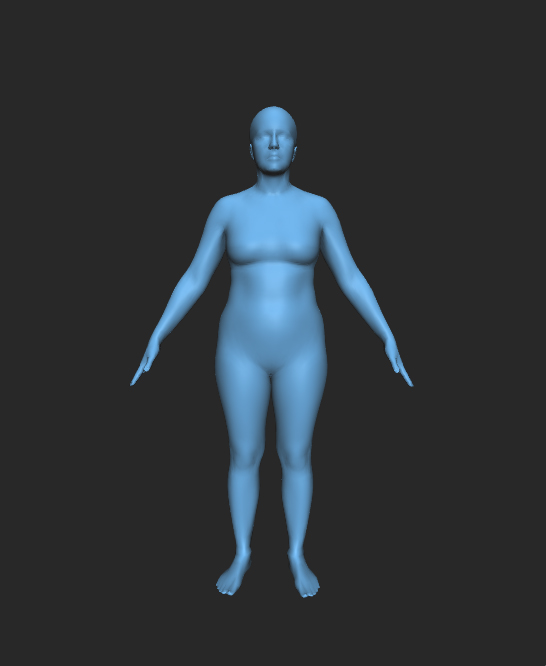
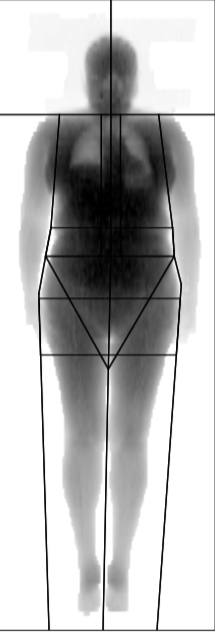
- BMI: 29.3 (grade 2 overweight)
- Waist: 94 (elevated according to WHO)
- WHR: 0.93 (elevated according to WHO)
- Total fat % from DXA: 41.9 (obesity)
- Abdominal region fat % from DXA: 50.2%
- Example of a non-obese BMI, with a very high fat percentage, elevated waist circumference, elevated WHR and very high abdominal region fat percentage.
- NOT OBESE ACCORDING TO BMI, INTRA-ABDOMINAL FAT VERY ELEVATED ACCORDING TO WHR AND DXA, ELEVATED CARDIOVASCULAR RISK
Patient nº5 (female)
- BMI: 38.6 (GRADE II obesity)
- Waist: 92 (elevated according to WHO)
- WHR: 0.72 (normal according to WHO)
- Fat % from DXA: 51.9 (obesity)
- Abdominal region fat % from DXA: 51.2%
- Example of an obese BMI, with a very high fat percentage, elevated waist circumference, elevated WHR and very high abdominal region fat percentage.
- OBESE ACCORDING TO BMI, INTRA-ABDOMINAL FAT VERY ELEVATED ACCORDING TO DXA BUT NOT ACCORDING TO WHR, ELEVATED CARDIOVASCULAR RISK
Patient nº6 (woman)
- BMI: 24.5 (normal weight)
- Waist: 75.5 (normal)
- WHR: 0.7 (normal according to WHO)
- Fat % from DXA: 33.4 (obesity)
- Abdominal region fat % from DXA: 32.5%
- Example of a normal BMI, with a high fat percentage, a normal waist circumference, normal WHR and a normal abdominal region fat percentage.
- NORMAL WEIGHT ACCORDING TO BMI, HIGH TOTAL FAT PERCENTAGE, INTRA-ABDOMINAL FAT NORMAL ACCORDING TO DXA AND WHR, NORMAL CARDIOVASCULAR RISK
Patient nº7 (woman)
- BMI: 29.8 (overweight)
- Waist: 87 (elevated)
- WHR: 0.79 (normal according to WHO)
- Fat % from DXA: 47 (obesity)
- Abdominal region fat % from DXA: 48%
- Example of a non-obese BMI, with a high fat percentage, elevated waist circumference, a normal WHR and high abdominal region fat percentage.
- OVERWEIGHT ACCORDING TO BMI, HIGH TOTAL FAT PERCENTAGE, INTRA-ABDOMINAL FAT NORMAL ACCORDING TO DXA AND WHR, NORMAL CARDIOVASCULAR RISK
BIBLIOGRAPHY
*Source: Spanish Society for the Study of Obesity (SEEDO 2007)
(1) Sahakyan, K., Somers, V., Rodriguez-Escudero, J.P. et al “Normal-Weight Central Obesity: Implications for Total and Cardiovascular Mortality” Ann Intern Med. Published online 10 November 2015 doi:10.7326/M14-2525
https://annals.org/article.aspx?articleid=2468805
(2) Poirier, P. “The Many Paradoxes of Our Modern World: Is There Really an Obesity Paradox or Is It only a Matter of Adiposity Assessment?” Ann Intern Med. Published online 10 November 2015 doi:10.7326/M15-2435.

