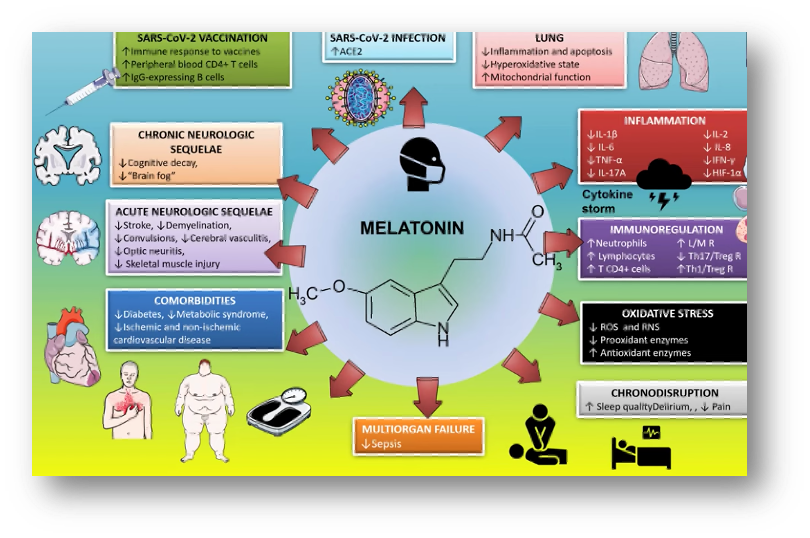
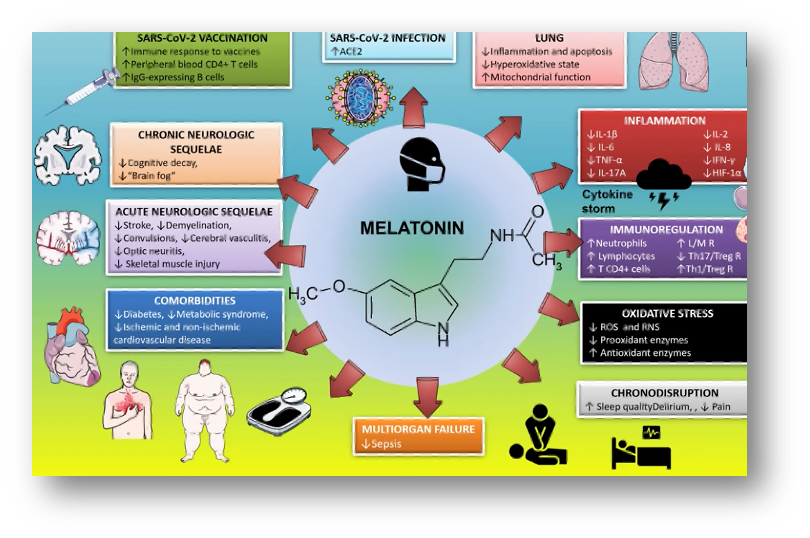
Melatonin is of great importance in COVID-19. In humans, its levels are reduced in DM2, metabolic syndrome, and cardiovascular disease, and its therapeutic value has been demonstrated.
The development of an effective vaccine is crucial to control the disease, especially in the elderly who present impaired immunity. Melatonin has been shown to stimulate the production of interleukin which increases the CD4+ lymphocyte population. Thus, its use in vaccination would enhance immune response, and its duration.
Dr. Alfonso Galán González – Neolife Medical Team
Introduction
In this second part of this series on melatonin and coronavirus, we will discuss the protective effects at the cellular and neuronal level specifically that this molecule has and how it can improve the outcome of vaccination. We’ll also provide some insights into two studies currently underway.
“Mental fog”, a term that describes a state of confusion, forgetfulness, inability to concentrate, fatigue, and low mental energy appears to be a major after effect of COVID-19 disease. In this context, the neuroprotective properties of melatonin deserve some consideration.
Cytoprotective effect
Type 2 diabetes (DM2), metabolic syndrome, and heart disease of ischemic or non-ischemic origin are comorbidities that aggravate COVID-19 disease. The prevalence of metabolic syndrome (a set of cardiovascular risk factors that include a larger waist circumference, high levels of triglycerides, high blood pressure, high glucose, and low HDL cholesterol) worldwide varies from 15 to 30% depending on the region and leads to a 1.5 to 2.5-fold increase in the risk of cardiovascular mortality. According to the CDC (Centers for Disease Control), people with metabolic syndrome are 10 times more likely to die from COVID-19.
And here lies the importance of controlling these diseases during the pandemic.
In humans, melatonin levels are reduced in DM2, metabolic syndrome, and cardiovascular disease, and its therapeutic value has been demonstrated in several studies with doses of 2 to 5 mg daily. In animal models of these diseases, it has demonstrated effectiveness in reducing symptoms. All cells in the body contain melatonin in quantities greater than the circulating melatonin produced in the pineal gland. It is synthesized in the mitochondria, but for unknown reasons this melatonin is not released into the extracellular space. Therefore, to improve intracellular melatonin levels we must use high doses of melatonin, much higher than those used as a chronobiotic agent. Allometric calculations indicate doses in the range of 40 to 100 mg per day for cytoprotective effects.
Neuroprotective effect
Various neurological after effects like anosmia, stroke, paralysis, cranial nerve involvement, encephalopathy, delirium, meningitis, and seizures have been observed in COVID patients. The cause may be the virus itself, thrombotic complications, or an exaggerated cytokine response. Antibodies in cerebrospinal fluid, white matter changes, and psychological and psychiatric consequences are found in these patients.
A study of over 84,000 British patients with varying severities of COVID-19 disease showed in those who were even asymptomatic – regardless of race, age, educational background, income level, or previous illness – a decline of about 10 years on average in global cognitive abilities. The so called “mental fog”, a term that describes this state of confusion, forgetfulness, inability to concentrate, fatigue, and low mental energy appears to be a major after effect of the disease. In this context, the neuroprotective properties of melatonin deserve some consideration.
In the early stages of cognitive decline, patients treated with melatonin show improved performance in several neuropsychological and depression tests, as well as improved sleep quality and ability to stay awake during the day.
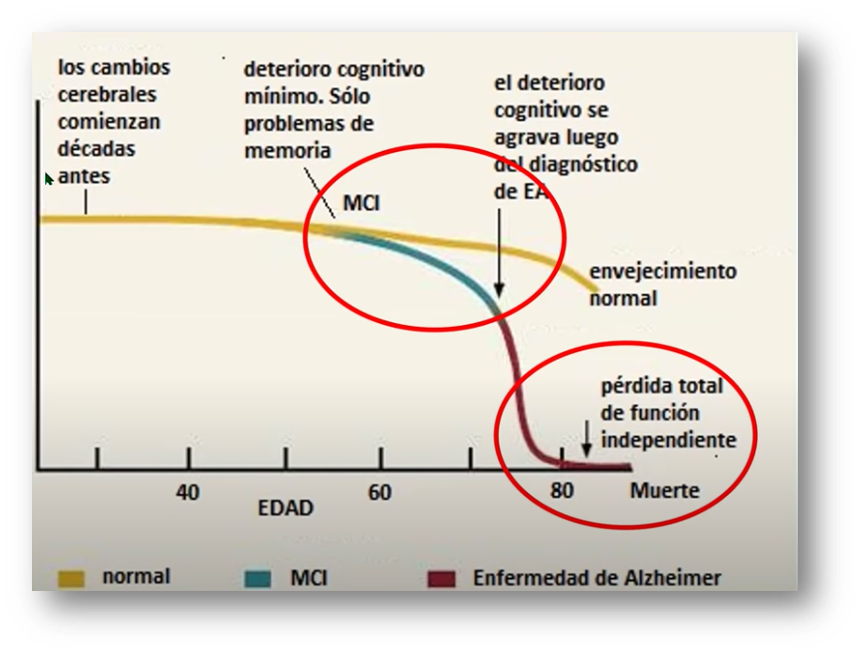
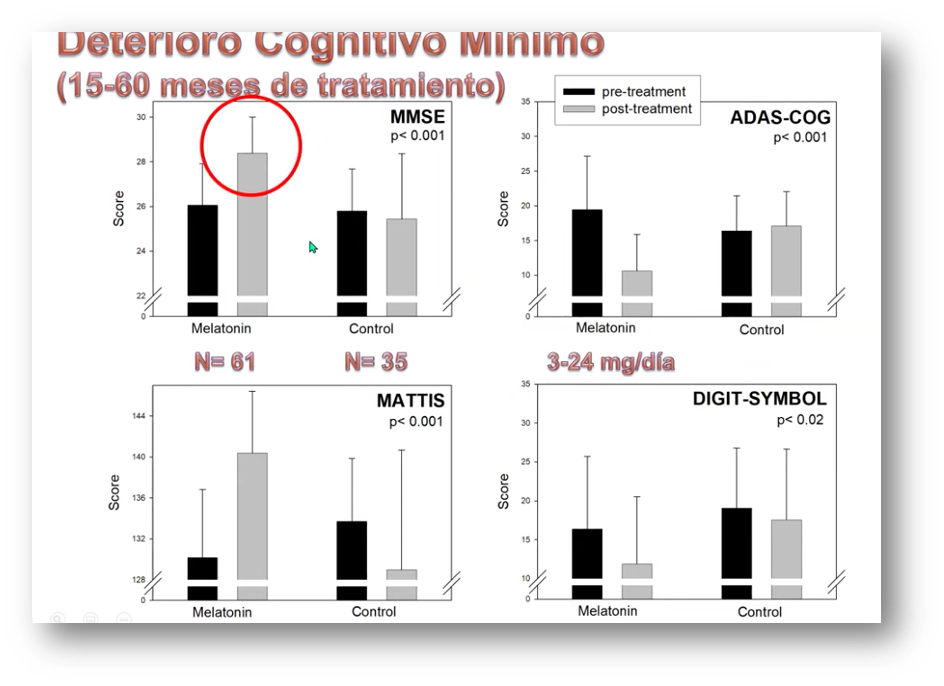
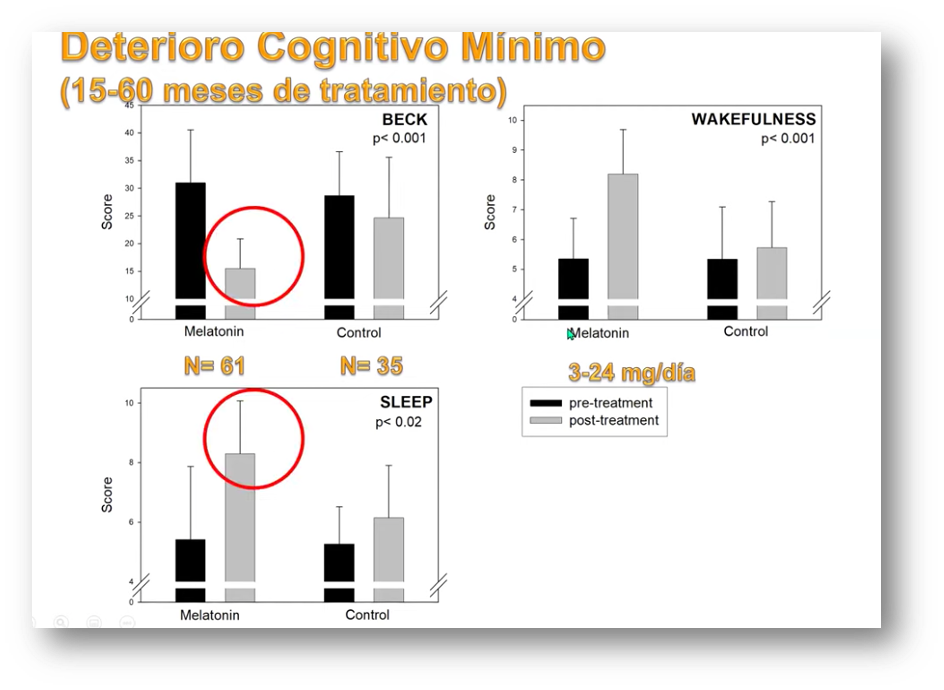
The thickness of the lamina cribrosa has been shown to be a marker of neurodegenerative diseases. Another recent study has shown how treatment with doses of melatonin of 0.15 mg/kg in minimal cognitive impairment increases its thickness as well as hippocampal volume, lowering CSF tau levels – a marker of cognitive impairment in cerebrospinal fluid – and improving the results of the Mini-Mental test.
Boosting effect of the vaccine
Initial data from vaccines already in use show some lower protection in older patients. Melatonin may help close that gap.
The existing literature indicates that:
- Melatonin is effective in counteracting the immunosuppression seen in aging, an effect produced by increasing CD4+ T lymphocytes.
- Melatonin is an adjuvant in cancer vaccinations by enhancing the response of CD8+ T lymphocytes (cytotoxic).
- Melatonin enhances the immune response to vaccines by increasing CD4+ T lymphocytes and B cells that produce IgG.
A recent study shows that plasma from convalescent COVID patients has a strong CD4+ response to the Spike protein, which is the target of current vaccines, and that this response was related to IgG and IgA levels.
In some patients, the immune response is not sufficient and cases of reinfection have been documented.
Thus the development of an effective vaccine is crucial to control the disease, especially in the elderly who show lower CD8+ cell counts due to inhibition of IL-2 and IL-2 receptors. Melatonin has been shown to stimulate the production of this Interleukin by increasing CD4+ cells. And so its use in vaccination would enhance the kind of immunity that the vaccine is trying to create by boosting the immune response and its duration over time.
This outline summarizes what we have discussed in these posts on melatonin and COVID.
Now we will present some of the highlights of two studies underway in Spain that seek to study different effects of melatonin in this disease.
Ongoing studies at the HULP (Hospital Universitario La Paz, Madrid) with melatonin in COVID-19
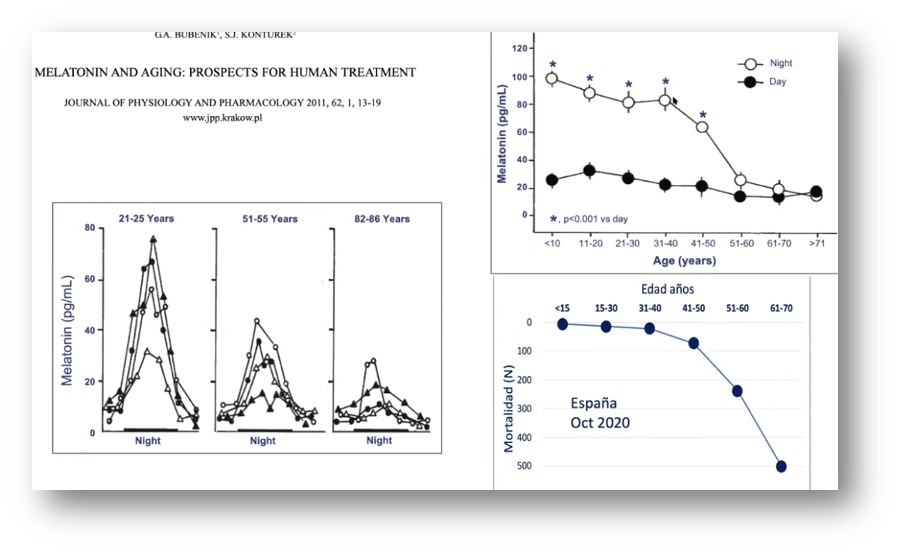
The first one we’ll mention seeks to find out if a low dose of melatonin (2 mg.) may prevent infection in high risk contacts and if patients taking it develop less severe disease. The logic behind this study lies in the observation that children have less severe COVID, and they have very high levels of melatonin. Is this what protects them from severe COVID?
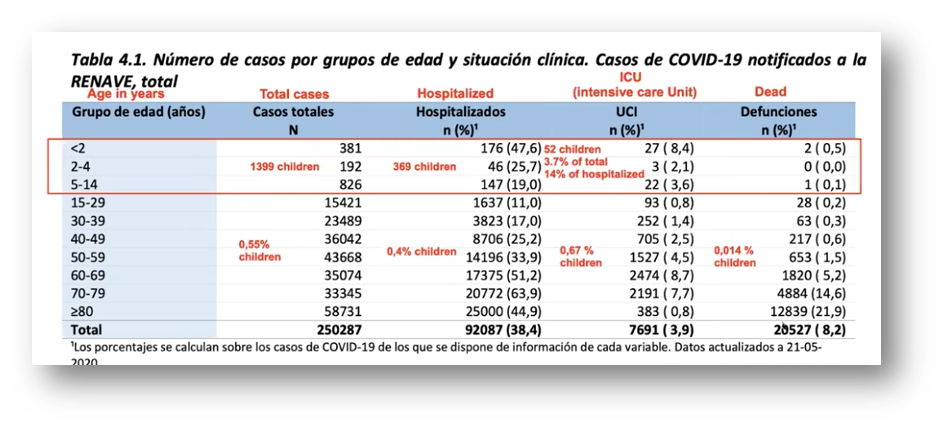
Women, as seen in these graphs, also present a lower mortality rate from COVID-19…and also have higher melatonin levels than men.
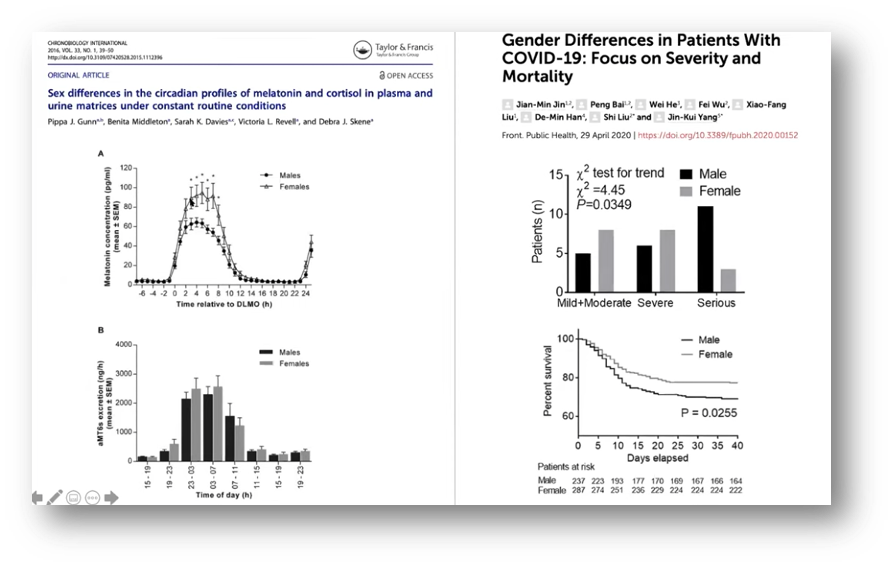
The other ongoing study seeks to find out if treatment with very high doses of melatonin in critically ill patients admitted to the ICU improves their prognosis. The available evidence shows that COVID mortality curves are very similar to those of melatonin level decline.
There are data that show that exposure to natural light improves the prognosis of patients with sepsis.
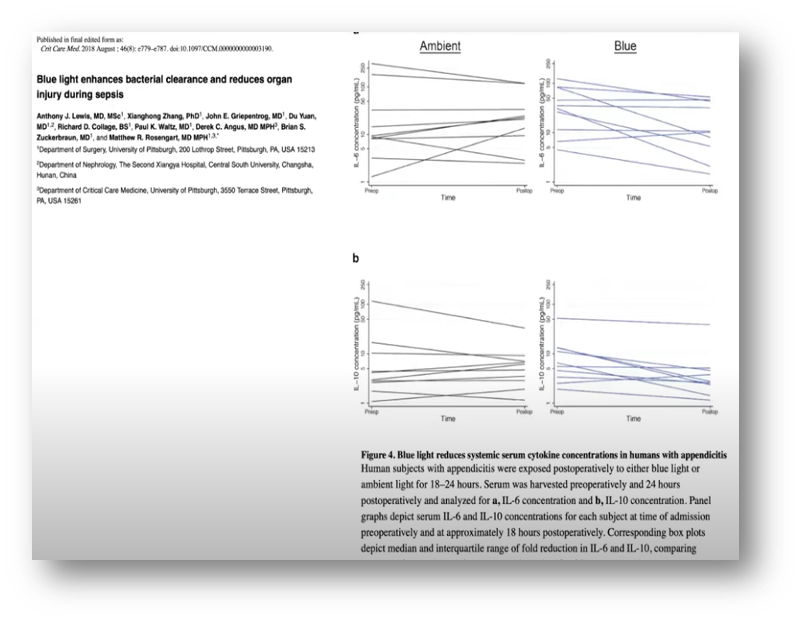
There is also growing evidence that melatonin has a very important effect on sepsis, inflammation, and immunity. Some examples:
These patients will receive intravenous melatonin in doses of 5 mg/kg every 6 hours for 7 days, and we will see if this decreases mortality, length of stay in ICU, need for ventilation, vital organ failure, and thrombotic phenomena.
BIBLIOGRAPHY
(1) Simko, F.; Hrenak, J.; Dominguez-Rodriguez, A.; Reiter, R.J. Melatonin as a putative protection against myocardial injury in COVID-19 infection. Expert Rev. Clin. Pharmacol. 2020, 13, 921–924.
(2) Cardinali, D.P. Melatonin: Clinical perspectives in neurodegeneration. Front. Endocrinol. 2019, 10, 480
(3) Cardinali, D.P.; Vigo, D.E.; Olivar, N.; Vidal, M.F.; Brusco, L.I. Melatonin therapy in patients with Alzheimer’s disease.Antioxidants 2014, 3, 245–277
(4) Cardinali, D.P.; Vigo, D.E.; Olivar, N.; Vidal, M.F.; Furio, A.M.; Brusco, L.I. Therapeutic application of melatonin in mild cognitive impairment. Am. J. Neurodegener. Dis. 2012, 1, 280.
(5) Xu, L.; Yu, H.; Sun, H.; Hu, B.; Geng, Y. Dietary melatonin therapy alleviates the lamina cribrosa damages in patients with mild cognitive impairments: A double-blinded, randomized controlled study. Med. Sci. Monit. 2020, 26, e923232-1.
(6) Cardinali, D.P.; Esquifino, A.I.; Srinivasan, V.; Pandi-Perumal, S.R. Melatonin and the immune system in aging. Neuroimmunomodulation 2008, 15, 272–278.
(7) Moreno, A.C.; Porchia, B.F.; Pagni, R.L.; Souza, P.D.C.; Pegoraro, R.; Rodrigues, K.B.; Barros, T.B.; Aps, L.R.; de Araújo, E.F.; Calich, V.L.; et al. The Combined Use of Melatonin and an Indoleamine 2,3-Dioxygenase-1 Inhibitor Enhances Vaccine-Induced Protective Cellular Immunity to HPV16-Associated Tumors. Front. Immunol. 2018, 9, 1914.
(8) Cardinali DP, Brown GM, Pandi-Perumal SR. Can Melatonin Be a Potential “Silver Bullet” in Treating COVID-19 Patients?. Diseases. 2020;8(4):44. Published 2020 Nov 26.