Pulse wave velocity (PWV) is now the most accurate tool for the early detection of arterial aging and for understanding when hypertension truly begins—even when office blood pressure values are still within the normal range.
Added to this is the value of the renin/aldosterone ratio, which allows us to identify the underlying mechanism driving blood pressure elevation in each individual and to personalize management with unprecedented precision. This is what hypertension looks like in 2026: true anticipation and treatment tailored to each patient’s physiology.
Dr. Carlos Martí – Neolife Medical Team
For years, hypertension was understood as a number: above 140/90 mmHg meant “disease”; below that threshold, “everything was fine.”
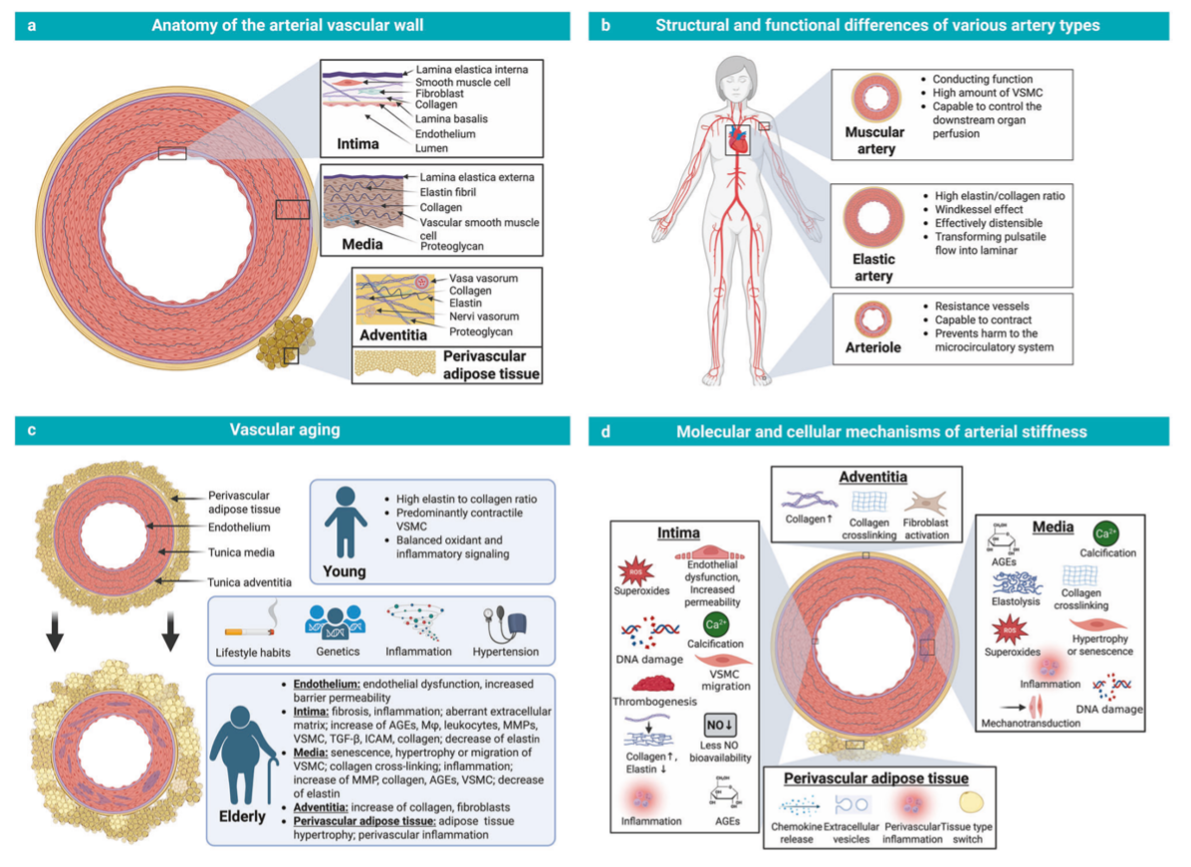
Today we know this approach is insufficient. The most recent evidence points to something more profound: elevated blood pressure is the late consequence of accelerated arterial aging—now recognized as vascular aging—which can be detected long before the blood pressure cuff shows abnormal values.
What truly matters is no longer just measuring blood pressure, but understanding what is happening inside the arteries during that silent phase that determines future risk, even when everything appears normal. This represents one of the most important evolutions of recent years: hypertension is no longer seen solely as a diagnosis, but as an opportunity for early detection. A paradigm shift that reshapes how we assess cardiovascular risk and opens the door to earlier, more precise intervention with a real capacity for long-term prevention.
Over the past decade, we have learned that:
- Vascular damage begins 5–10 years before blood pressure readings become elevated.
- Arterial stiffness predicts real cardiovascular risk more accurately than brachial blood pressure.
- Many individuals with “normal–high” blood pressure already show signs of arterial aging.
For this reason, the latest updates prioritize the assessment of vascular physiology rather than interpreting numbers alone.
Arterial stiffness: the first “surname” of hypertension
One of the parameters that has gained the most relevance in recent years is pulse wave velocity (PWV), an essential marker of arterial stiffness. Understanding it is simple if we imagine our arteries as household pipes: when they are new, flexible, and well maintained, they absorb pressure and allow smooth flow. Over time, as they become stiffer, each pressure wave travels faster and with greater force.
PWV measures exactly how fast the pressure wave travels along the aorta.
When this wave travels too quickly, the artery has lost elasticity. And this can occur years before blood pressure rises. In other words, a person may have “normal blood pressure” and yet already display the first surname of future hypertension: increased arterial stiffness, indicating premature vascular aging.
SphygmoCor: measuring what very few can
Assessing arterial stiffness cannot be done with a conventional blood pressure monitor. At Neolife, we use SphygmoCor, the international reference technology used in advanced cardiovascular research.
This highly validated system allows us to:
- Accurately measure PWV.
- Calculate central blood pressure, which is the pressure that truly loads the heart and brain.
- Determine whether a patient’s arterial stiffness is appropriate for their age or reflects accelerated vascular aging.
This technology, although widely validated, is still largely limited to centers with an advanced approach to vascular assessment. Its true value lies in its ability to detect alterations during the silent phase, when intervention is still both effective and highly personalized.
This is the foundation of true prevention—not merely reactive care.
RAAS and the renin/aldosterone ratio: the second surname of hypertension
In recent years—and particularly in the most recent updates—the renin/aldosterone ratio has gained greater importance, as it allows us to go beyond blood pressure values and understand the internal mechanism driving blood pressure elevation in each individual.
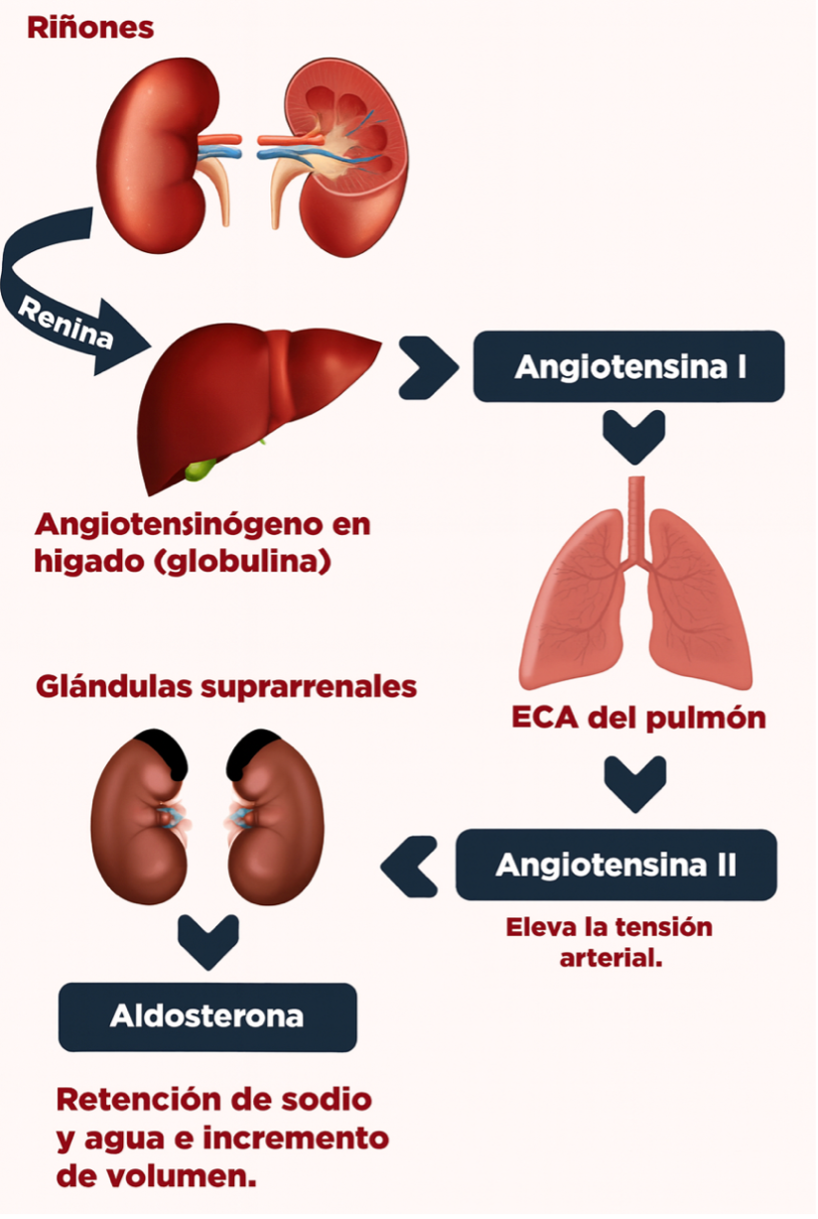
The RAAS (renin–angiotensin–aldosterone system) is the body’s mechanism for regulating blood pressure, salt balance, and fluid volume. It functions as an internal blood pressure thermostat: when the body perceives insufficient pressure or volume, it activates the system to raise it; when there is excess, it suppresses it.
- Renin is the initial signal, released when the body detects low pressure or volume.
- Renin triggers the formation of angiotensin, which constricts arteries and rapidly increases blood pressure.
- Angiotensin then stimulates the release of aldosterone, a hormone that promotes sodium and water retention, increasing circulating volume and sustaining elevated blood pressure.
By analyzing the renin/aldosterone ratio, we can identify which part of the system is altered—essentially determining the physiological mechanism pushing blood pressure upward in that specific individual. This is key to personalizing treatment and identifying the “second surname” of hypertension: whether there is excessive system activation, aldosterone predominance, or abnormally low renin levels.
This approach allows us to move away from the uniform “one-size-fits-all” strategy. While some profiles clearly benefit from ACE inhibitors or angiotensin II receptor blockers (ARBs), others respond better to calcium channel blockers, beta-blockers, aldosterone antagonists, or even targeted supplementation and lifestyle optimization strategies.
Lifestyle in 2026: interventions that truly rejuvenate the vasculature
New guidelines emphasize something we know well at Neolife: not all lifestyle recommendations impact arterial health in the same way. Certain interventions directly improve arterial stiffness and central blood pressure.
Resistance training combined with high-intensity intervals improves aortic elasticity more effectively than moderate exercise alone. Reducing visceral fat decreases hemodynamic load and improves central pressure.
Achieving deep, stable sleep—particularly restoring the normal “dipper” pattern—acts as a powerful nocturnal cardiovascular protector.
The dipper pattern refers to the natural nighttime reduction in blood pressure, typically around 10–20%. When this decline does not occur, cardiovascular risk increases significantly. It is assessed through 24-hour ambulatory blood pressure monitoring (ABPM), which tracks blood pressure behavior during sleep.
Importantly, these changes are not applied intuitively, but through a personalized approach: identifying the dominant mechanism in each individual and directing lifestyle interventions toward that specific target.
Because hypertension is not prevented with generic advice, but by optimizing arterial physiology through precise and measurable interventions.
The true antiaging approach: acting before disease appears
Traditional medicine diagnoses hypertension once blood pressure crosses a defined threshold. Longevity medicine prefers to intervene when physiology begins to deviate—before pathological numbers appear—helping the body return to its natural, physiological balance.
If a patient already shows a first surname (increased arterial stiffness), a second surname (altered RAAS), or even rising central blood pressure, we are facing an early but still manageable process. This is the window of opportunity to get ahead of arterial aging and prevent long-term complications.
That is the Neolife approach: anticipate, identify early changes, and act with precision to keep arterial health on its youngest possible trajectory.
BIBLIOGRAPHY
(1) Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, Muiesan ML, Tsioufis K, Agabiti-Rosei E, Algharably EAE, Azizi M, Benetos A, Borghi C, Hitij JB, Cifkova R, Coca A, Cornelissen V, Cruickshank JK, Cunha PG, Danser AHJ, Pinho RM, Delles C, Dominiczak AF, Dorobantu M, Doumas M, Fernández-Alfonso MS, Halimi JM, Járai Z, Jelaković B, Jordan J, Kuznetsova T, Laurent S, Lovic D, Lurbe E, Mahfoud F, Manolis A, Miglinas M, Narkiewicz K, Niiranen T, Palatini P, Parati G, Pathak A, Persu A, Polonia J, Redon J, Sarafidis P, Schmieder R, Spronck B, Stabouli S, Stergiou G, Taddei S, Thomopoulos C, Tomaszewski M, Van de Borne P, Wanner C, Weber T, Williams B, Zhang ZY, Kjeldsen SE. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023 Dec 1;41(12):1874-2071.
(2) McEvoy JW, McCarthy CP, Bruno RM, Brouwers S, Canavan MD, Ceconi C, Christodorescu RM, Daskalopoulou SS, Ferro CJ, Gerdts E, Hanssen H, Harris J, Lauder L, McManus RJ, Molloy GJ, Rahimi K, Regitz-Zagrosek V, Rossi GP, Sandset EC, Scheenaerts B, Staessen JA, Uchmanowicz I, Volterrani M, Touyz RM; ESC Scientific Document Group. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. Eur Heart J. 2024 Oct 7;45(38):3912-4018.
(3) Herzog MJ. Arterial stiffness and vascular aging: mechanisms, clinical implications, measurement and future perspectives. Signal Transduct Target Ther. 2025;10:23.
(4) Adler, G. K., Brown, J. M., Vaidya, A., Calhoun, D. A., Carey, R. M., Funder, J. W., Stowasser, M., & the Endocrine Society. (2025). Primary Aldosteronism: An Endocrine Society Clinical Practice Guideline. Journal of Clinical Endocrinology & Metabolism. , ePub ahead of print.
(5) Manual MSD.