Osteoarthritis is better known than arthritis, but this pathology affects at least 300 million people in the world and has a very important impact on quality of life and mortality.
Osteoarthritis is a disease that is still being studied; we may develop it after a trauma or because we have an “inflammatory activation”. The manifestations (areas and degree of involvement) may vary from one individual to another. What is clear is that this disorder affects every element of the joint.
Dr. Celia Gonzalo Gleyzes – Neolife Medical Team
Osteoarthritis (OA) is a serious disease
OA is the most prevalent arthritic problem in the global population over 60 years of age, generally affecting knees, hips, spine, and fingers.
Pain is the first symptom, the one that leads the individual to consult a doctor and the reason, sometimes, for incapacity.
The diagnosis is established by a combination of clinical history, physical examination, and imaging test findings. Blood tests are requested to rule out other diseases.
OA pain is neuropathic and central.
The causes of pain are not completely clear; let us not forget that cartilage is aneural (it lacks nerves), but the bone and synovial membrane can produce stimuli or respond to them, causing painful sensations.
Osteoarthritis is a disease that can limit our daily life (inability to work and even to walk; at this point, I would associate an increase in mortality).
OA, a disease that affects the entire joint
This pathology leads to joint destruction, starting with cartilage degradation. It therefore affects the cartilage, synovial tissue, subchondral bone, tendons, and ligaments. The main players in the onset of the problem are the cartilage, the subchondral bone, and the synovial membrane. These tissues secrete signaling molecules (cytokines) that control the degeneration of the articular cartilage matrix.
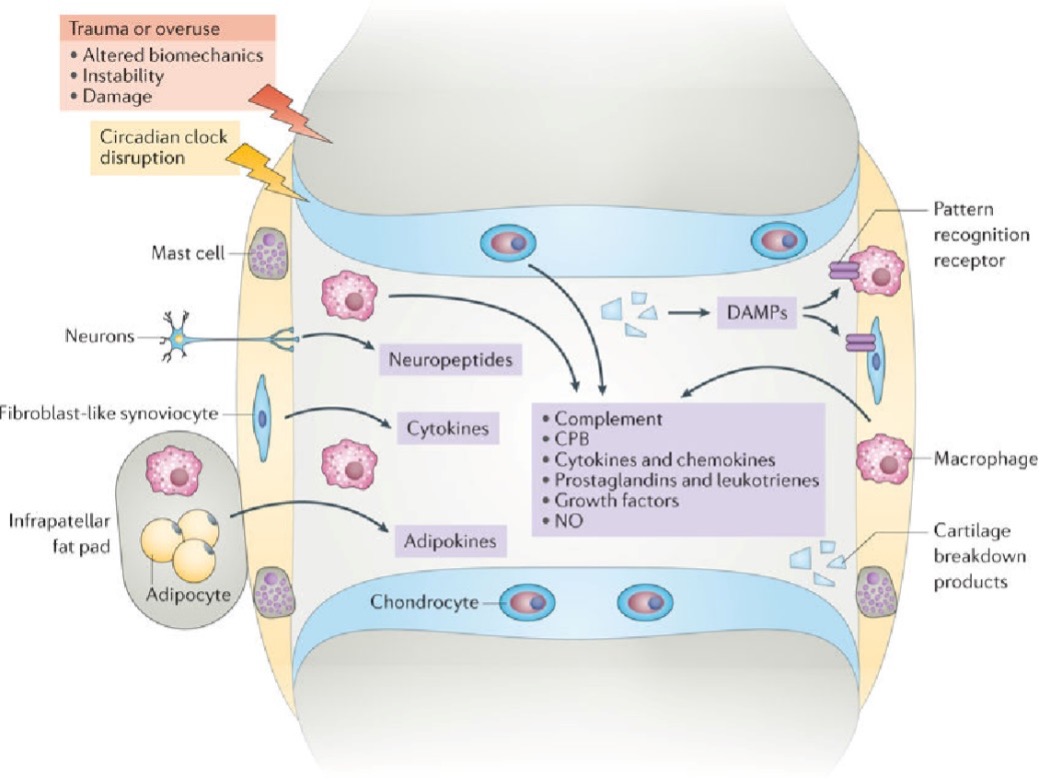
The effects of proinflammatory cytokines in OA outweigh the anti-inflammatory effects of other cytokines and growth factors; the joint homeostatic balance is disrupted. This causes the cartilage and bone to degrade, new pathological bone to form, and the osteophytes and the synovial membrane to become inflamed (synovitis).
In some patients, the inflammatory process begins when bits of degraded cartilage come into contact with the synovial tissue. When this tissue becomes inflamed, even more degradative and inflammatory mediators (cytokines, lipid mediators, neuropeptides, and matrix metalloproteinases (MMPs)) are secreted. These mediators cause the chondrocytes (cartilage cells) to produce more MMPs, thereby degrading more cartilage and promoting a vicious inflammatory cycle. Remodeling of the subchondral bone is observed and may even involve the bone marrow. The subchondral bone may also synthesize more inflammatory mediators that contribute to joint degradation.
Synovitis is a potential predictor of structural progression of medial compartment osteoarthritis. The degree of synovitis (in patients without established OA) is sometimes predictive of the patient’s cartilage loss (before it is seen in imaging).
Various origins and presentations of osteoarthritis
Osteoarthritis is a complex pathology whose development may already be preprogrammed by events in early adulthood and adolescence.
There are different phenotypes (expressions of the disease) that can help us to establish a more focused treatment:
- Based on the affected part of the body (hand, knee, hip, spine)
- Based on etiology (origin): obesity/metabolic syndrome, aging, post-trauma, genetics, etc.
- Based on distribution: generalized vs. localized
- Based on the degree of pain
- Initial vs advanced
- Primary vs secondary
- Based on the affected tissues
We will focus our attention on three phenotypes:
- Post-traumatic
The disease is triggered following trauma/damage to any joint tissue (ligaments, synovial tissue, subchondral bone or cartilage). Meniscal fragments or anterior cruciate ligament injuries increase the risk of osteoarthritis, more so if they occur concomitantly.
Innate immunity is particularly important in this process. Joint damage may damage the extracellular matrix, releasing fragments of it that will be recognized by Toll-like receptors. Elevated levels of Toll-like receptors and their ligands are present in cartilage lesions characteristic of osteoarthritis.
- Caused by aging
Inflammation, cellular aging, production of oxygen free radicals lead to increased oxidative stress and chondrocyte aging.
Cellular senescence can be replicative or secretory. There may be chondrocytes with low replication, but with mediator secretion capacity. The problem occurs when they exhibit a senescence-associated secretory phenotype (SASP), i.e. characterized by the secretion of proinflammatory factors.
Oxidative stress contributes to the reduced mitochondrial biogenesis observed in chondrocytes of osteoarthritis patients. A reduction of AMPK (enzyme that detects nutrients and regulates cellular energy metabolism) may also occur, which influences mitochondrial biogenesis and ultimately the repair capacity of chondrocytes.
In an interesting animal model with OA, it was observed that the elimination of senescent (aged) chondrocytes reduced pain and increased the production of new cartilage.
- Metabolic
The link between obesity and osteoarthritis in weight-bearing joints (knee and hip) has been widely demonstrated. In fact, when patients lose weight, pain and swelling decrease.
The curious thing is that patients with obesity also present a higher incidence of OA of the interphalangeal joints of the hands; this is due to the fact that adipose tissue produces inflammatory mediators, the adipokines. Obesity is also associated with increased intestinal permeability and dysbiosis; metabolites such as lipopolysaccharide (LPS) pass from the gastrointestinal tract into the bloodstream causing low-grade inflammation.
To sum up, metabolic syndrome alters bone remodeling, increases synovial and intra-articular fat inflammation, and increases cartilage catabolism (destruction).
Type 2 diabetes mellitus is also a risk factor for OA (1).

Combating osteoarthritis
After reading these lines, we may deduce that any person could develop this limiting disease that may lead to joint replacement or poly-medication.
It is obvious that slowing down aging, engaging in an adequate and balanced sports activity (avoiding injuries, with supplementation, adapted sports advice, practicing complementary sports), fighting obesity/overweight, controlling cardiovascular risk factors (blood pressure, lipids, and carbohydrate metabolism), treating intestinal dysbiosis (through microbiota studies) are the keys to combating osteoarthritis. One more reason to start taking care of yourself with the help of Neolife.
BIBLIOGRAPHY
(1) Berenbaum F, Walker C. Osteoarthritis and inflammation: a serious disease with overlapping phenotypic patterns. Postgrad Med. 2020 May;132(4):377-384. doi: 10.1080/00325481.2020.1730669. Epub 2020 Feb 26. PMID: 32100608.
(2) Imagen: Robinson, W., Lepus, C.M., Wang, Q., Raghu, H., Mao, R., Lindstrom, T., & Sokolove, J. (2016). Low-grade inflammation as a key mediator of the pathogenesis of osteoarthritis. Nature Reviews Rheumatology, 12, 580-592.

