Overweight and obesity have been linked to an increased incidence of lung diseases, such as asthma, chronic obstructive pulmonary disease (COPD), or sleep apnea syndrome. Recent research links this pathology with severe forms of COVID-19, increasing the health risk of worsening the disease.
The natural history of chronic noncommunicable diseases, such as obesity, is the result of the combination of genetic factors, a sedentary life, and unhealthy eating. A new study published in the prestigious scientific journal The Lancet has called overweight and obesity the main risk and severity factor in the COVID-19 process.
Tania Mesa – Director of Neolife Nutrition and Nursing Unit
Excess fat is associated with an inflammatory state that may be increased by infection with the virus.
Obesity and all chronic noncommunicable diseases represent the true global pandemic. Cases of obesity have almost tripled between 1975 and 2016 worldwide. Overall, about 13% of the world’s adult population (11% of men and 15% of women) were obese in 2016 (1). The new SARS-CoV-2 coronavirus, which produces the disease known as COVID-19, continues to expand rapidly around the world. This is a respiratory virus that has been shown to be transmitted quite easily and puts this group of people at greater risk.
The Spanish Society for the Study of Obesity (SEEDO) states that almost half of the Spanish population, subjected to several weeks of lockdown, has experienced an increase in their average weight during this period of time (2). The results of his recently published survey indicate that 44% of the population claims to have gained weight during lockdown and, the majority, 73%, report a weight gain range of between 1 and 3 kilos. Half of the population surveyed in the SEEDO study was unaware that obesity worsens the prognosis of those who have COVID-19 (2).
Increasingly, we have data that point to overweight and obesity as factors linked to a poor prognosis in patients infected with COVID-19. Older age is the main indicator of mortality, but COVID-19 disease affects all ages. Recently, a clear inverse correlation between age and body mass index (BMI) has been shown, in which people admitted to the hospital were more likely to be obese and suffer acute forms of the novel coronavirus disease (3. 4). In a report by the UK’s Intensive Care National Audit and Research Centre (ICNARC), which includes 2,621 patients in intensive care units (ICUs) with COVID-19, 30.7% had a BMI of 30-40, and 7% was higher than 40. With regard to prognosis, the chance of survival was higher in patients with a BMI that was lower than 30 (5).
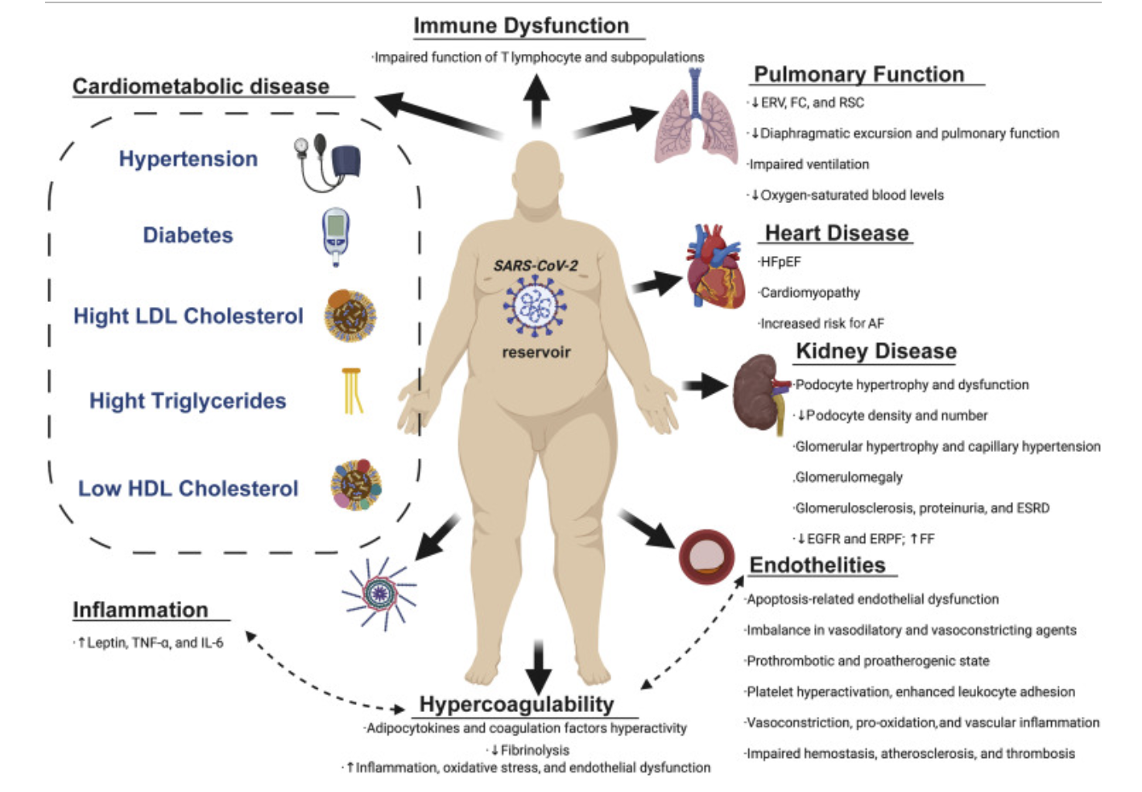
A new review published by the Mayo Foundation for Medical Education and Research shows that respiratory infections are more common in overweight patients. Obesity is associated with a decrease in respiratory reserve volume and functional capacity of the respiratory system. Generally, the obese patient has a higher number of pro-inflammatory cytokines (proteins responsible for intercellular communication) associated with excess fat tissue. Subjects with obesity therefore present a pro-inflammatory environment and COVID-19 is expected to further exacerbate inflammation by exposing them to higher levels of circulating inflammatory molecules compared to thin subjects (Figure 1). This situation results in metabolic dysfunction, which may lead to dyslipidemia, insulin resistance, cardiovascular disease, high blood pressure, and type 2 diabetes (6. 7).
Another common feature in obesity is vitamin D deficiency, which increases the risk of infections and impairs immune response. By contrast, vitamin D supplements may prevent respiratory infections through various immunoregulatory functions, including decreased production of pro-inflammatory cytokines, reducing the risk of pneumonia. Vitamin D deficiency may be involved in the link between obesity and increased susceptibility to complications and mortality due to COVID-19 (7, 8). It should be noted that alterations in the gut microbiota are common in obese subjects and some protocols for the treatment of COVID-19 include the use of probiotics to maintain the balance of bacterial populations and thus strengthen the immune system (8).
The Massachusetts General Hospital points out that obesity is not a risk factor for becoming infected with COVID-19. However, obese patients are more likely to require intensive care for COVID-19 (9). A characteristic complication of obesity is hypoventilation syndrome, where excess fatty tissue from the chest wall makes it difficult for obese patients to breathe deep and completely. They point out that this combination increases the severity of symptoms in those who develop COVID-19.
Obesity is a chronic disease that requires treatment. A new study published in The Lancet magazine reminds us of the importance of acquiring healthy lifestyle habits. They emphasize that this is a good time to start taking steps towards losing 5% to 10% of your body weight if you are obese (10). Regarding diet, a normal protein low-calorie diet that is low on carbohydrates and fats may be a promising strategy for losing weight and improving health; however, the patient’s profile and condition should always be considered.
In short, there are several biological mechanisms by which COVID-19 disease may affect people with obesity to a greater extent. The treatment of obesity requires a multidisciplinary vision, since it is a complex and multifactorial disease, in which an important component is the balance between energy intake and expenditure, but there are also other contributing factors, such as food availability, age, gender, genetics, metabolism, and physical activity. It is important to note that there are other environments to consider, such as home quarantines, isolation by areas or neighborhoods, isolation due to close contact with patients with COVID-19, etc., as we have recently witnessed. Therefore, it is important for us to be aware of all these factors and to remember the data and information on the increase in body weight during the lockdown suffered in March.
Performing a global assessment, interpreting information, establishing treatment strategies, identifying modifiable factors, and individualizing treatment is what we do here at Neolife, thanks to our team of healthcare professionals and the great success stories we’ve obtained. Treatment should be initiated with the recommendation of lifestyle changes, which requires nutritional intervention, cognitive behavioral therapy, and specific exercise prescription, associated with the pharmacological treatment of obesity and its complications.
BIBLIOGRAPHY
(1) (2020). “Obesity and overweight”. World Health Organization.
URL: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
(2) SEEDO. (2020). “Un 44% de los españoles aumentaron de peso durante el confinamiento” [44% of Spaniards gained weight during lockdown]. Spanish Society for the Study of Obesity.
URL:https://www.seedo.es/images/site/notasprensa/NP_Un_44_de_espan%C3%9Eoles_ha_au
mentado_de_peso_durante_el_confinamiento_Ok.pdf
(3) Simmonnet, A. et al. (2020). “High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation”. Obesity. Vol. 28(7):1195-1199.
URL: https://pubmed.ncbi.nlm.nih.gov/32271993/
(4) Bellido G., D. (2020). “Obesidad y Covid-19. La relación cada vez más consistente” [Obesity and COVID-19: An increasingly consistent relationship]. Hospital Universitario de Ferrol. Spain.
(5) Fernández B., E. (2020). “Obesidad” [Obesity]. Píldora Científica. Revista Española de Salud Pública.
URL:https://www.mscbs.gob.es/biblioPublic/publicaciones/recursos_propios/resp/revista_cdrom/
Suplementos/Pildoras/pildora14_obesidad.pdf
(6) Sanchis-Gomar, F. et al. “Obesity and outcomes in COVID-19: when an epidemic and pandemic collide”. Mayo Clinic. Vol. 95(7): 1445-1454.
URL:https://www.sciencedirect.com/science/article/pii/S0025619620304778
(7) Chiappetta, S. et al. (2020). “COVID-19 and the role of chronic inflammation in patients with obesity”. International Journal of Obesity. Vol. 44, 1790-1792.
URL:https://www.nature.com/articles/s41366-020-0597-4
(8) Petrova, D. et al. (2020). “La obesidad como factor de riesgo en personas con COVID-19: posibles mecanismos e implicaciones” [Obesity as a risk factor in people with COVID-19: possible mechanisms and implications]. Atención Primaria. Vol. 52(7):496-500.
URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7247450/pdf/main.pdf
(9) Fitch, A. & Hutter, M. (2020). “Understanding links between COVID-19 and obesity”. Massachusetts General Hospital.
URL: https://www.massgeneral.org/digestive/weight-center/understanding-links-between-covid-19-and-obesity
(10) Rubino, F. et al. (2020). “Bariatric and metabolic surgery during and after the COVID-19 pandemic: DSS recommendations for management of surgical candidates and postoperative patients and prioritization of access to surgery”.
URL:https://www.thelancet.com/journals/landia/article/PIIS2213-8587(20)30157-1/fulltext
