More and more cases are being reported of patients who present clinical manifestations weeks or even months after they developed a coronavirus infection and have been considered cured. How long does coronavirus disease or COVID-19 last? Is there a post-acute, long, or even chronic COVID-19?
A significant number of patients affected by coronavirus disease present symptoms at the time of diagnosis. However, some of these clinical manifestations remain weeks or months after the patient is considered cured. Post-acute COVID-19 or long COVID-19 are terms that were coined to reflect a multi-system disease that persists after an acute illness due to this virus.
Dr. Débora Nuevo Ejeda – Neolife Medical Team
What is post-acute COVID-19?
There is currently no clear consensus on the exact definition of the clinical picture, but we may define it as the presence of symptoms after 3 weeks and up to 12 weeks after the onset of the first symptom.
After this period of 12 weeks since the presentation of the symptoms, perhaps the term to be used would be “chronic COVID-19”, although due to the recent nature of the pandemic, we do not yet have enough data to talk about chronicity in these terms.
Is post-acute COVID-19 common?
The data collected differ in the various studies carried out in different countries.
About 10% of patients confirmed as positive for SARS-CoV-2 infection in the UK continue to say they don’t feel well after 3 weeks.
In Italy, up to 87.4% of patients claim to have at least one or more symptoms, the most common being fatigue (53.1%), shortness of breath (43.4%), joint pain (27.3%), and chest pain (21.7%).
In the USA, only 65% of those affected consider their health returned to what it had been prior to infection.
Why do some people continue having symptoms?
The reason why some people take longer to recover compared to others is still unknown.
Persistent long-term presence of virus in the blood, weakness, or the absence of antibodies, as well as relapses or “reinfections,” factors dependent on inflammatory or autoimmune response, a lack of physical fitness, and psychological factors, such as post-traumatic stress, may help prolong the symptoms.
Long-term respiratory, musculoskeletal, and neuropsychiatric sequelae have already been described for other coronaviruses such as SARS and MERS, and a clear pathological parallelism may be traced to post-acute COVID-19.
What are the symptoms?
The symptomatic variety within what we call post-acute COVID-19 is very wide. The most commonly described symptoms are cough, low fever, and fatigue. These typically disappear and reappear, becoming intermittent.
Other clinical manifestations afflicting these patients include shortness of breath, chest pain, headaches, neurocognitive difficulties, muscle weakness and pain, gastrointestinal problems, rash and other skin lesions, metabolic disorders (such as difficulties controlling diabetes), thromboembolic phenomena, depression, and various consequences at the mental health level.
Skin conditions may vary greatly including maculopapular lesions, hives, or an injury in the limbs that looks like chilblains (which has already been called the “COVID foot”).
What studies or tests can be helpful in long COVID-19?
The most important thing is a correct assessment carried out by a trained professional. A good medical history that collects symptoms, as well as the onset and duration of those symptoms is essential.
Likewise, an adequate and individualized physical examination of each system, that evaluates the possible alterations or sequelae caused by COVID-19 as it passes through the body, will also guide the diagnosis and help us decide whether or not additional complementary tests are needed.
Blood tests should be prescribed specifically for each patient depending on each clinical case. Among the most useful and easier to access, and therefore most indicated by the responsible healthcare professionals are:
- Blood tests that should include:
- Complete blood count: Hemoglobin levels to assess the presence of anemia as the leading or adjuvant cause of shortness of breath. White blood cell count, as a reduced amount of white blood cells may be an indication of severity, as well as a low platelet count, while a high white blood cell count may be alerting us to the presence of acute infection and/or a secondary inflammatory response.
- Biomarkers such as the C-reactive protein may indicate acute infection; high levels of ferritin warn us of an inflammatory and prothrombotic state; troponin signals myocardial damage at the coronary or heart muscle level (myocarditis); and high levels of D-dimer may indicate the presence of a thromboembolic phenomenon.
- A chest x-ray should be performed on all patients who present respiratory symptoms, both for diagnosis and follow-up at 12 weeks, and it should be repeated if there are new or repeated respiratory symptoms.
In patients who present persistent alterations in the chest x-ray or in oxygen saturation levels as measured by a pulse oximeter, a low-dose chest CT scan should be indicated. The use of this test has spread to all follow-up consultations, as the radiation is not as high as that in a conventional x-ray and yet the information provided is more accurate and allows for evolutionary comparisons given the measurement and processing systems that are being protocolized.
- Pulmonary rehabilitation/therapy: in cases where there is evidence of alteration in any of the respiratory tests, it has been shown that initiating early respiratory physiotherapy helps these patients recover functional capacity.
What do we do now? Monitoring and management of long COVID
Long COVID-19 is a multi-system disease that requires patient management from a global perspective, understanding and attending the patient as a whole. Comorbidities or pathologies prior to or concomitant with COVID (such as diabetes, high blood pressure, kidney or cardiovascular disease) should be taken into account.
Providing a global vision and medical care, but which is also personalized and tailored to each circumstance, is the key. And this is our philosophy in our clinical practice at Neolife.
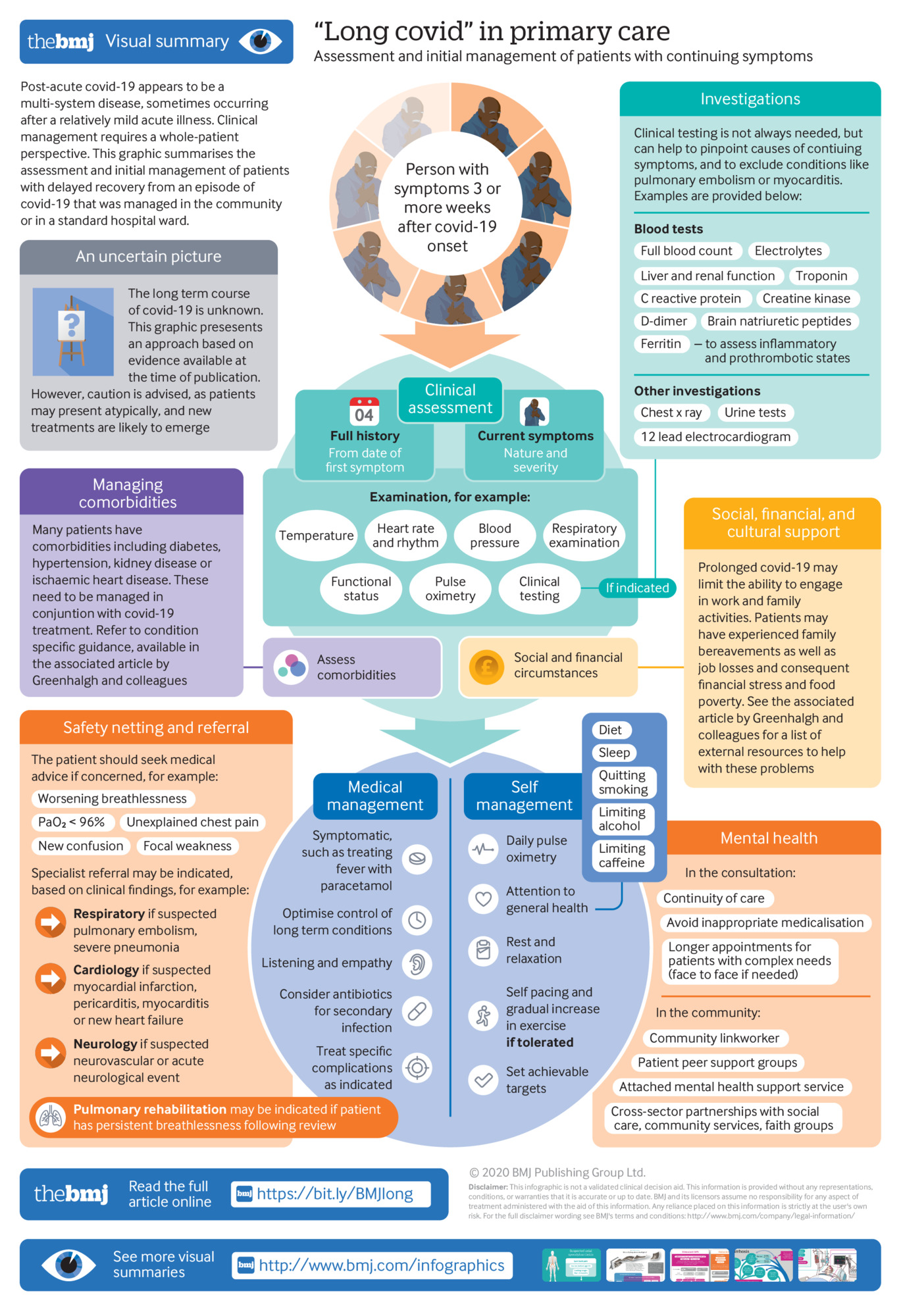
In an upcoming article, we will try to present step by step, and symptom by symptom, the possible solutions that may be provided to cure, prevent, or mitigate this so-called long or post-acute COVID, which is summarized in the following infographic.
BIBLIOGRAPHY
(1) Carfì A, Bernabei R, Landi F, for the Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020;324(6):603–605. doi:10.1001/jama.2020.12603
(2) Geddes L. Why strange and debilitating coronavirus symptoms can last for months.New Scientist 2020. https://www.newscientist.com/article/mg24632881-400-why-strange-and-debilitatingcoronavirus
(3) Trisha Greenhalgh, 1 Matthew Knight, 2 Christine A’Court, 1 Maria Buxton, 3 Laiba Husain1.Management of post-acute covid-19 in primary care. BMJ 2020;370:m3026 https://dx.doi.org/10.1136/bmj.m3026 Published: 11 August 2020
(4) Assaf G, Davis H, McCorkell L, et al. An analysis of the prolonged COVID-19 symptoms survey by Patient-Led Research Team. Patient Led Research, 2020. https://patientresearchcovid19.com/.
