Erectile dysfunction is defined as the persistent inability to achieve or maintain an erection that allows for satisfactory sexual intercourse.
Having good testosterone levels is critical to having satisfactory erections, but there are many more factors involved. It can happen for vascular, neurogenic, anatomical, hormonal, drug-induced or psychogenic reasons. In many cases more than one cause is to blame.
Dr. Alfonso Galán González – Neolife Medical Team
Epidemiological data reveal a high incidence and prevalence of erectile dysfunction globally.
Erectile dysfunction (ED) is defined as the persistent inability to achieve or maintain an erection that allows for satisfactory sexual intercourse.
Epidemiological data reveal a high incidence and prevalence of erectile dysfunction globally. The Massachusetts Male Aging Study (MMAS) indicates a prevalence of 52% (to varying degrees) among men between the ages of 40 and 70 in the New England region. In a German study on men between the ages of 30 and 80, however, the prevalence was 19.2%, with a very significant increase with age from 2.3% to 53.4%. A Dutch study of men in consultation for erectile dysfunction observed that 1 in 4 were under the age of 40, and half of them reported severe erectile dysfunction.
To better understand the causes that can lead to erectile dysfunction, we’re going to look at what phenomena must occur for a man to have a satisfactory erection.
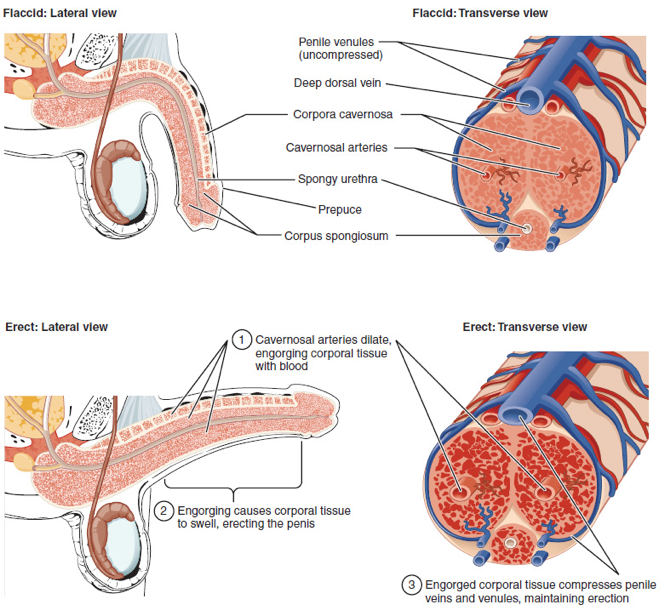
An erection occurs when 2 tubular structures, the corpora cavernosa that run all the way through the penis and the corpus spongiosum containing the urethra, fill with blood. This can occur due to a series of physiological stimuli such as arousal and sexual stimulation, processes with a strong hormonal influence, especially testosterone.
In the presence of mechanical stimulation, the erection is initiated by the parasympathetic nervous system (a division of the autonomic, unconscious or voluntary, nervous system). These parasympathetic nerve branches range from the sacral plexus to the arteries that reach the erectile tissue. When stimulated, acetylcholine is secreted, which causes the release of nitric oxide, a vasodilator agent. Thus the arteries dilate and fill the corpora cavernosa with blood.
The next step is preventing that blood from receding. The ischiocavernosus and bulbous muscles compress the veins, preventing the blood from being drained. After ejaculation or the cessation of stimulation, parasympathetic stimulation disappears and the blood leaves the corpora cavernosa through the venous system.
The cerebral cortex, i.e. our superior, more advanced brain functions, can initiate erection in the absence of stimulation in response to visual stimuli, olfactory stimuli, imagination, etc. They operate through erection centers in the sacral and lumbar regions of the spinal cord. Moreover, the cerebral cortex can suppress erection, even in the presence of mechanical stimulation, as can other environmental, psychological or emotional factors.
Erection can also occur spontaneously at night, in a process that is believed to be mediated by the brainstem during the REM sleep phase and is thought to be a form of “maintaining” the proper health of our erections. The presence or not of these nocturnal erections has diagnostic value.
In view of this, we can understand the large number of mechanisms required for an erection to occur and the large number of steps at which it can fail. Erectile dysfunction can occur for vascular, neurogenic, anatomical, hormonal, drug-induced or psychogenic reasons. In many cases more than one cause is to blame.
- Vascular:
- Habits (smoking).
- Sedentary lifestyle and lack of exercise.
- Obesity.
- Cardiovascular disease (high blood pressure, coronary heart disease, peripheral artery disease, etc.).
- Diabetes, dyslipidemia, metabolic syndrome, hyperhomocysteinemia, etc.
- Pelvic surgery sequelae (prostatectomy or radiation therapy).
- Neurogenic:
- Main causes:
- Degenerative diseases (multiple sclerosis, Parkinson’s, etc.).
- Spinal diseases or trauma.
- Stroke.
- CNS tumors.
- Peripheral causes:
- Diabetes.
- Kidney failure, liver failure.
- Polyneuropathy.
- Pelvic surgery with nerve damage.
- Urethral surgery.
- Main causes:
- Anatomical or structural:
- Hypospadias, epispadias.
- Peyronie’s disease.
- Penile cancer or other external genital tumors.
- Hormonal:
- Diabetes mellitus; metabolic syndrome.
- Hypogonadism.
- Hyperprolactinemia.
- Hyper and hypothyroidism.
- Hyper and hypocortisolism.
- Multiple endocrine disorders.
- Mixed mechanisms:
- Chronic illness.
- Psoriasis, gouty arthropathy, ankylosing spondylitis, hepatic steatosis, chronic periodontitis, glaucoma, inflammatory bowel disease, etc.
- Iatrogenesis.
- Drug side effects:
- Antihypertensive drugs (thiazides, beta blockers, etc.).
- Antidepressants.
- Antipsychotics.
- Antiandrogens (GNRH analogues, 5-alpha-reductase inhibitors).
- Drug abuse (alcohol, heroin, cocaine, marijuana, methadone, synthetic drugs, anabolic steroids, etc.).
- Psychogenic:
- Generalized type (lack of arousal or sexual intimacy disorders).
- Situational type (related to the relationship, with execution or with stress).
- Trauma.
- Penis fracture.
- Pelvic fractures (1).
Diagnosing the particular cause of erectile dysfunction requires careful medical evaluation, with detailed anamnesis on habits, history, illnesses, drug taking, specific sexual questionnaire, psychiatric or emotional symptoms, etc. A physical examination of the area checking for deformities, prostate exam, signs of hormonal, vascular or neurological disease. A complete analytical study with blood count, hormone levels (free testosterone, dehydroepiandrosterone, estradiol, prolactin, etc.) and metabolic parameters and cardiovascular risk.
The study can be completed with more specific tests such as the doppler ultrasound of the penis with provocation tests or nocturnal tumescence testing. This test is important because if the patient is able to have erections at night we can assume that the vascular and neurological mechanisms are working and the cause is more likely psychogenic.
What can be done?
Treatment will ideally be aimed at correcting the suspected cause of erectile dysfunction. It is based on hygienic-dietary measures and modification of habits, pharmacological measures, physical therapy and finally surgical therapies to restore flow or implantation of prostheses.
- Modification of harmful lifestyle habits is fundamental and should be considered prior to other therapeutic approaches and treatments. These include:
- Quitting smoking.
- Drinking in moderation.
- Get a good night’s sleep.
- Good dietary habits. Monitoring the intake of sugars and saturated fats and increasing the consumption of vegetables.
- Performing regular exercise. 30 minutes, 5 times a week. Some studies show benefits from performing pelvic floor exercises (Kegel) (2).
- Encourage communication and trust with your partner.
- More and more pharmacological measures are becoming available to improve blood flow to the penis such as sildenafil and Tadalafil or Alprostadil.
- Newer treatments such as the use of shock waves to stimulate the creation of new blood vessels and improve flow are yielding very promising results.
And perhaps in a class of its own, straddling the line between lifestyle changes and pharmacology, is the hormone replacement therapy with bioidentical hormone that we have developed at Neolife. This therapy is very helpful and is primarily aimed at achieving adequate physiological levels of DHEA and testosterone. The Massachusetts Male Aging Study looked at the correlation of 17 hormones and erectile dysfunction and found that only DHEA had a negative relationship (i.e. greater dysfunction at lower levels). This led researchers to study its effect on this pathology in detail. Reiter et al. showed improvements in erectile dysfunction, satisfaction during coitus, sexual desire and orgasmic function after 16 weeks of use (3). Meanwhile, treating male hypogonadism by replenishing testosterone levels has been shown in several recent meta-analyses to improve erectile function, sexual desire and orgasmic function (4).
The conclusion that we want to convey here at Neolife is that erectile dysfunction is a multi-factor clinical picture that must be evaluated and treated from multiple axes, hormonal therapy being a very important one, but still just one of them.
BIBLIOGRAPHY
(1) https://uroweb.org/guideline/male-sexual-dysfunction/#3
(2) Dorey, G. , Speakman, M. J., Feneley, R. C., Swinkels, A. and Dunn, C. D. (2005), Pelvic floor exercises for erectile dysfunction. BJU International, 96: 595-597
(3) Reiter WJ, Pycha A, Schatzl G, Pokorny A, Gruber DM, Huber JC, et al. Dehydroepiandrosterone in the treatment of erectile dysfunction: a prospective, double-blind, randomized, placebo-controlled study. Urology 1999;53:590–4.
(4) Corona G, Rastrelli G, Morgentaler A, Sforza A, Mannucci E, Maggi M. Meta-analysis of Results of Testosterone Therapy on Sexual Function Based on International Index of Erectile Function Scores. Eur Urol. 2017 Dec;72(6):1000-1011.
