Obesity and being overweight are related to genetic, biological, social, socioeconomic and environmental factors. In recent decades, several studies suggest that the gut microbiota is another factor associated with the development of this pathology.
It is widely accepted that metabolic disorders, such as obesity, are closely related to lifestyle and diet. Now, groups of researchers and new research such as the European MyNewGut project, are assessing how diet can influence gut microbiota and thus modify our metabolic and mental health.
Tania Mesa – Director of Neolife’s Nutrition and Nursing Unit
Alejandro Monzó- Neolife Nutrition and Nursing Unit
We are what we eat
The term microbiota denotes a set of microorganisms that reside in a given environment. Human beings have groups of bacteria in different parts of our body: in the skin, in the mouth, in the gastrointestinal tract and in the vagina, among others.
Our gut microbiota contains 100 billion microorganisms, including at least a thousand different species of bacteria that comprise more than 3 million genes, 150 times more than in the human genome. In fact, the gut microbiota can weigh up to 2 kilograms. One third of our microbiota is common to that of the majority, while the other two thirds are specific to each individual (1).
The gut microbiota provides essential functions for human beings. Three primary functions have been identified, which are, generally, functions of nutrition and metabolism, protection functions and trophic functions on the proliferation and differentiation of the intestinal epithelium, as well as the development and modulation of the immune system. Some of these functions are (1):
- Helping the body to digest certain foods that the stomach and small intestine are not able to digest.
- Contributing to the production of certain vitamins (B and K).
- Helping to combat the aggressions of other microorganisms, by maintaining the integrity of the intestinal mucosa.
- It plays an important role in the immune system, acting as a barrier effect.
The development of the gut microbiota begins at birth. Its composition evolves throughout our entire life, from birth until we get older, and at the same time is influenced by a host of environmental factors.
Environmental factors such as the increase in calorie intake and the decrease in the physical activity have been considered as causing the increase in the prevalence of obesity and Metabolic diseases. However, nutrition plays a key role in the development of healthy or, on the contrary, harmful microbial populations. This is confirmed by a review published by the magazine Genes & Nutrition. Growing evidence suggests that the gut microbiota is an important factor contributing to the individual’s response to nutrients (2).
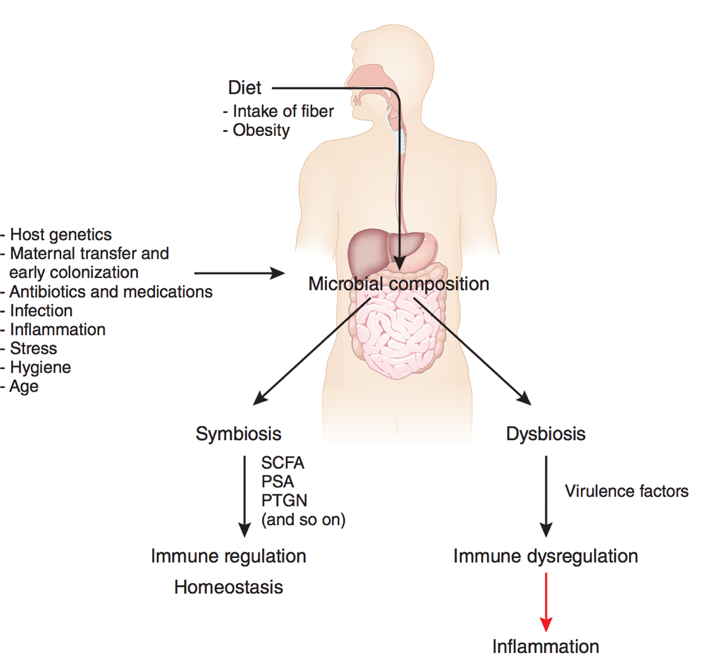
The human gut microbiota can be considered as being an organ within another organ (the digestive system) that has evolved with humans to achieve a symbiotic relationship that leads to physiological balance, and has been called our second genome or second brain. Researchers point out that the human being provides an environment rich in nutrients, and the microbiota offers indispensable functions that humans can’t perform by themselves. That said, it has been shown that the gut microbiota regulates the energy metabolism and storage of fat, and researchers believe it is a driving force in the development of metabolic disorders associated with obesity (Figure 1) (2).
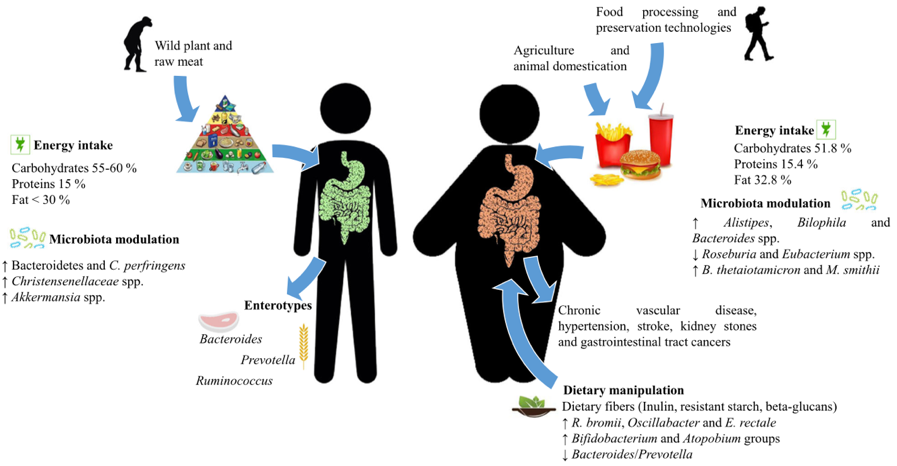
Therefore, the permanent interaction between gut microbiota and the human body opens a door to research into its relationship with diseases. The authors note that diet significantly influences the composition of the gut microbiota. Diet not only has the capacity to act on the immune system directly, but also indirectly, by modulating the gut microbiota, whose composition and metabolites may influence the individual’s health. Alterations of the gut microbiota and the adverse response of the individual to these changes is known as dysbiosis (Figure 2) (2,3).
On the other hand, a European project known as MyNewGut has conducted a five year study into the relationship between gut microbiota and its genome in the development of obesity and disorders linked to behavior with regard to our lifestyle. As conclusions, the researchers point to the following (4):
- The bacterial strains in our intestine could be the next generation of probiotics.
- The consumption of an excess of proteins generates certain toxic metabolites.
- Diets rich in fibers are associated with fewer symptoms of depression, help maintain body weight and reduce the risk of developing chronic metabolic diseases.
- A diet high in fat can have a negative impact on the gut microbiota and on the brain.
- The gut microbiota influences metabolic health.
At this point, the Western diet, characterized by being high in unhealthy fats, refined flours, sugars and salt, and low in dietary fiber, can contribute to a dysbiosis in the gut microbiota. This fact leads to an alteration in the bacterial populations, while in turn predisposing to obesity and chronic diseases (2,3). The MyNewGut project also demonstrates that certain microorganisms, such as Bacteroides Uniformis or Bifidobacterium Pseudocatenulatum have the capacity to reduce obesity, modify oral glucose tolerance and, most surprisingly, influence the mood of the individual, specifically the depression associated with obesity. The goal is clear, to develop other strategies, such as the identification of bacteria or bioactive metabolites, and use them as probiotics (4).
At Neolife, we consider our patients’ gut microbiota to be important, detecting those cases in which it is altered and working to keep it balanced and healthy.
BIBLIOGRAPHY
(1) Gut Microbiota for Health. 2019; 9:1–12. “Información sobre la microbiota intestinal”. URL: https://www.gutmicrobiotaforhealth.com/es/informacion-sobre-microbiota-intestinal/
(2) Duranti S. and others. (2017). “Obesity and microbiota: an example of an intricate relationship”. Genes & Nutrition. Italy. 1-15 URL: https://www.ncbi.nlm.nih.gov/pubmed/28638490
(3) Maslowski K.M. y Mackay C.R. (2011). “Diet, gut microbiota and immune responses”. Nature Immunology. Vol. 12, No1, pp: 1-5 URL: https://www.ncbi.nlm.nih.gov/pubmed/21169997
(4) (2019). “The Microbiome’s influence on energy balance, brain development, diet-related diseases and behavior”. European Union. URL: https://www.mynewgut.eu/sites/default/files/MyNewGut%20Leaflet_project_results%2B.pdf

