The importance of a high VO2max is increasingly being recognized as the first diagnosis of good health and longevity, far beyond the common values.
Peak oxygen consumption normally has an exclusive focus on performance, but according to the latest research, obtaining a high value means the absence of disease and the assurance of good health in the future.
Dr. César Montiel – Neolife Medical Team
When we want to know our state of health, we usually use a medical check-up that includes blood pressure, heart rate, BMI, fat %, and blood tests to control the levels of sugar, triglycerides, transaminases, and cholesterol, and sometimes even spirometry and electrocardiogram at rest.
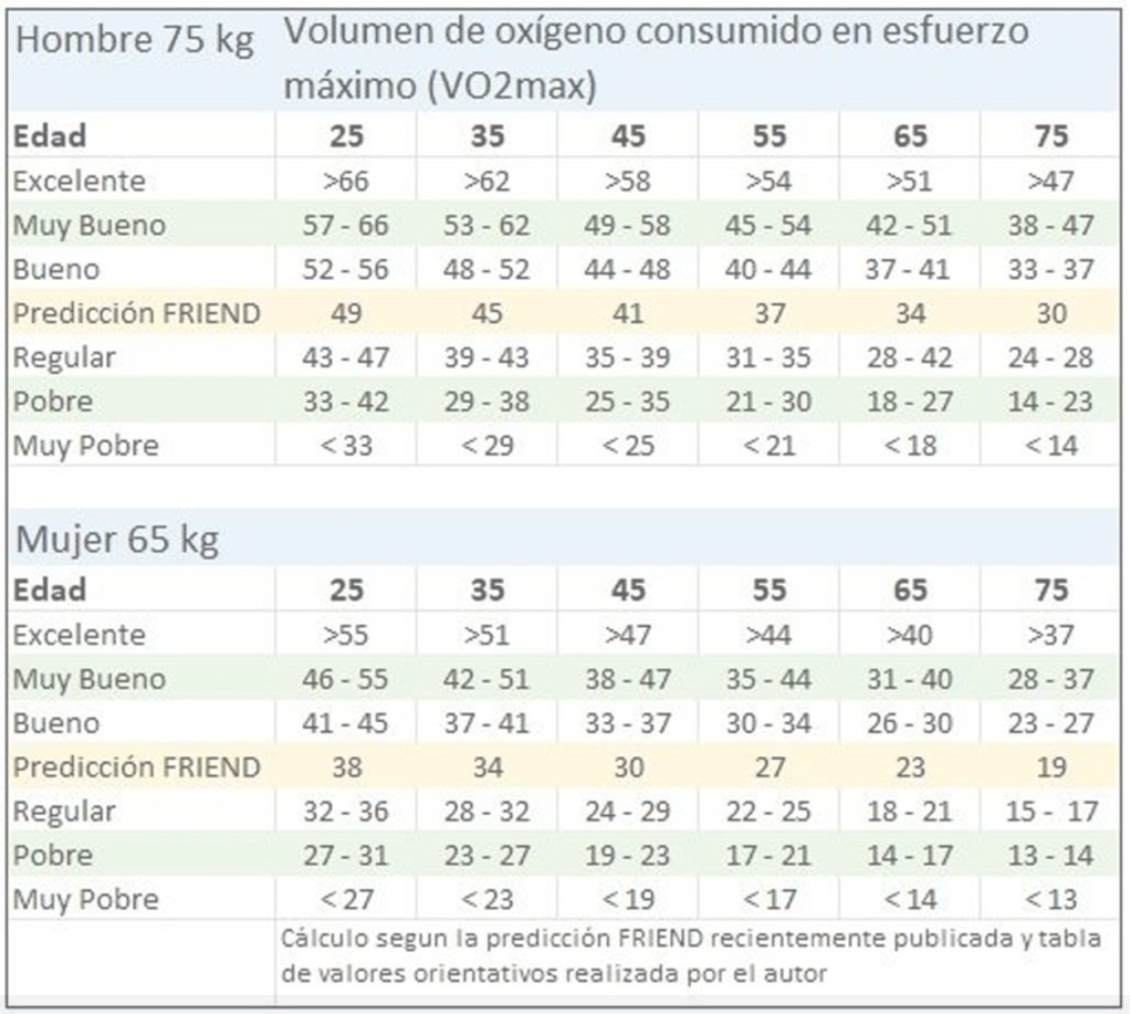
However, the importance of a high VO2max is increasingly recognized as the first diagnosis of good health and longevity, well above the previous assessments; even the American Heart Association considers it necessary to perform a stress test every year and considers the assessment of VO2max the “gold standard” of health.
Peak oxygen consumption normally has an exclusive focus on performance, but according to the latest research, obtaining a high value means the absence of disease and the assurance of good health in the future. Even longitudinal studies have shown that an increase of only 1 ml/kg/min reduces all-cause mortality by 11%, cardiovascular disease by 15%, and cancer by 16%.. The survival rate in a serious event (work accident, traffic accident, etc.) is much higher for those with higher metabolic efficiency.
Recent research has provided a reference for predicting VO2max adjusted for age and weight. So if you are above this average, you have a very significant assurance of good health.
What does it mean to have metabolic flexibility?
Currently, there is a growing interest in assessing the influence of metabolic flexibility, which can be defined as the ability of a system to adjust fuel oxidation to fuel availability. In other words, to have the capacity to quickly use the substrate that will allow us to have energy available, based on availability and need, or in other words, to have the capacity to use glucose in moments of intense activity with a limited duration and fatty acids for moments of less intensity and rest (stored in our adipocytes), which is what we have been designed for over the course of millions of years, and so, in this way, to always have energy available.
All this will depend on the type and amount of nutrients available for oxidation at the cellular level, and so people with good metabolic flexibility will have better body fat oxidation and optimal sports performance. Having food easily and readily available at all times is not natural, nor is not having to move to get it, as the vast majority of today’s jobs are very inactive. But it’s also unnatural to eat 5 or more times a day, and if this food is processed (many kcal that do not generate satiety and are extremely easy to digest), this leads to the obesity epidemic we are currently living in.
However, the new way of life in developed societies has generated a phenomenon that is not accepted by our genes and triggers health problems. We have evolved over thousands of years, but in a very short time we have created a world for which our body is not prepared, full of comforts and without stimuli. We have lost our Metabolic Flexibility (MF), and in the long run, this makes us sick.
Our muscle mass, liver, and adipose tissue are the great energy reservoirs, since they govern Metabolic Flexibility in a direct relationship with the endocrine system, so any alteration of this control may attract pathologies linked to the opposite, the dreaded Metabolic Inflexibility, which is present in people who have insulin resistance, diabetes, and obesity.
What happens when we eat?
The postprandial phase begins, where the body must decide what to do with each macronutrient ingested, in other words, use it as fuel or store it. It’s a complex process, but let’s explain it this way:
We can’t store alcohol, it must be burned immediately, and this inhibits the use of other substrates, interfering with the burning of fat and with the proper functioning of the liver.
Ingested protein has mainly a structural role (building muscle, hormones, neurotransmitters, etc.), although it may also be used in part as fuel. Surplus protein can’t be stored directly; it must first be converted into glucose through a process called gluconeogenesis.
We also have carbohydrates that are converted into glucose, a fuel that can be used by any cell and easily stored in the form of glycogen (in muscles or the liver). If the available reserves are exceeded, glucose can also be stored as fat.
Last but not least, dietary fats can be used as energy, for structural tasks (cell membranes, hormones…) or stored directly as subcutaneous or intramuscular fat.
Imagine that the food you ate had X amount of calories and 60% was ultimately stored. A process called partitioning will occur, (some of those calories are stored as muscle, as protein or muscle glycogen) and some as fat. This depends partly on what you have eaten, but also on your metabolic flexibility. Once this selection phase is over, the post-absorptive phase begins, which is where you start to use the reserves, and it will not end until you eat again.
Partitioning also occurs, but as output; if you expended 50% of your calories in this post-absorptive phase, how many came from glycogen and how many from fat?
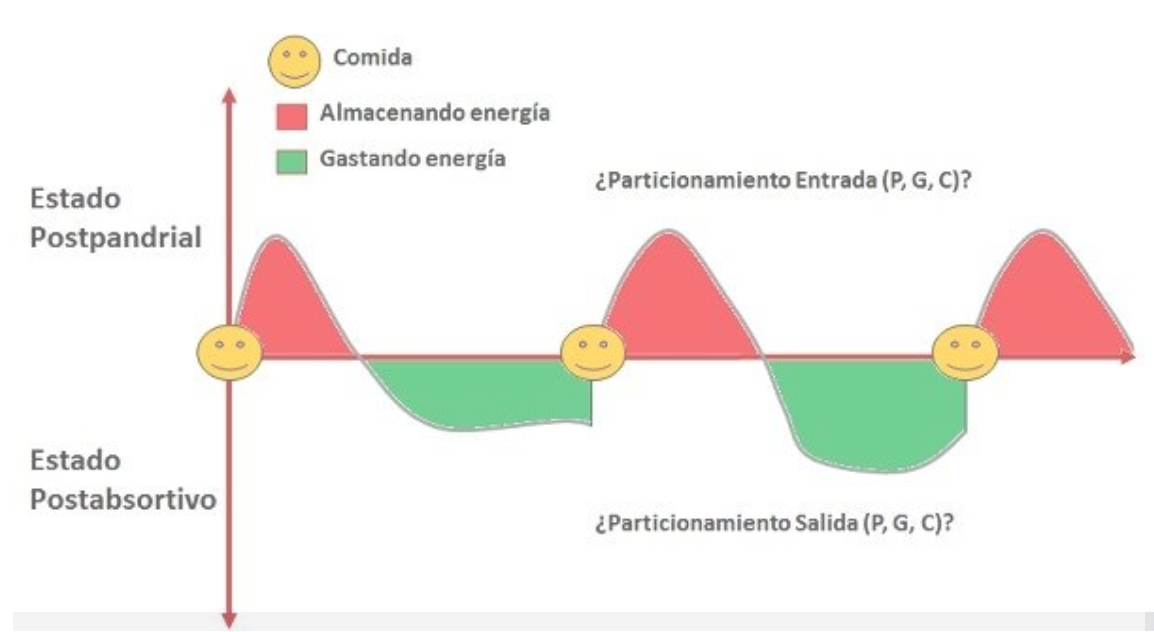
The graph tells us that our weight is determined by the differences in energy, i.e. the energy expended and stored, but your body composition (muscle/fat ratio) will depend on the partitioning of input compared to output.
This must be:
- In the postprandial state, we store almost all excess energy as muscle (protein + glycogen).
- In the post-absorptive state, we obtain almost all the energy required from stored fat, reserving glycogen for occasional high intensity efforts.
How do we find out if we have the right metabolic flexibility?
It is simpler than you think, and there is no need for blood tests or complex studies. Simply complete a period of fasting on an active day (more than 14-16h) and exercise at medium/low intensity. If you don’t feel any discomfort or dizziness (hypoglycemia) in these conditions, when glycogen stores are low, it is very likely that you were able to consume a large part of the energy used in the form of fatty acids. But if every time you don’t eat for 4-5h, you feel sick, there’s a problem, because it is an indication of metabolic inflexibility and future metabolic problems, even if you have blood tests that are within the normal range.
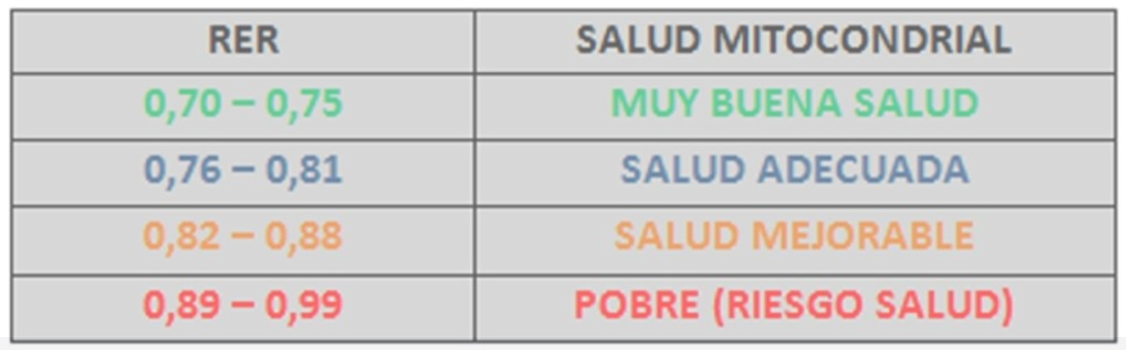
There are other methods that could provide us with more specific values of metabolic flexibility such as the FAST MAX test, where after a fast of 5 to 6 hours, if you have high blood sugar levels, you will use this as the main source of energy because you have extra. We will then perform a gas analysis measurement at rest and during exercise, increasing the intensity progressively until reaching the anaerobic threshold. That is to say, it will not be demanding since we don’t need to reach maximum intensities as in a stress test; in this case, we will be able to see the CO2 you produce and the O2 you consume, and it would give us a Respiratory Exchange Ratio (RER) as a result, which tells us quite precisely the percentage of nutrients that serve as a source of energy.
Although there is a lot of research on performance, there is very little on the normal population and health. But more and more research is being done on the consumption of fats in different types of subjects and their health benefits.
The differences between a person with high and low metabolic flexibility are maintained 24 hours a day. This means that consuming more or less fat is constant, at rest and during exercise, and even the response at meals is different. Having a better metabolic flexibility means benefits in health, but also in terms of appearance, since it is much easier to reduce the percentage of fat.
In a few years’ time, future blood tests will not measure good and bad cholesterol, something that has already been shown not to have much influence on health. Occupational medical check-ups will be much more useful by radically changing the way of assessing patients to anticipate illnesses that for now can only be seen when they are already present. Here at NEOLIFE, we already use more useful means such as measuring the level of cellular oxidation and Redox potential to control metabolic damage and all mitochondrial diseases (type 2 diabetes, arteriosclerosis, obesity, cancer, neurodegenerative diseases, etc.), or a stress test to assess RER and VO2max, among others.
Knowing how we use oxygen by knowing its volume and the oxidation capacity of our mitochondria is the best way to know more about our metabolic health, something that NEOLIFE wants you to know is highly recommended. If we complete a stress test once a year, trying not to decrease our VO2max (since it is the best reference), and knowing how to use nutrients, we could control our metabolic flexibility on a regular basis, and in this way we would be able to maintain healthy values (RER 0.8 or lower); this would indicate that we are able to use fats as a nutrient and we have an adequate insulin sensitivity.
Don’t miss Part 2 of this article, where we will cover the tools to improve these areas.
BIBLIOGRAPHY
(1) Bret H. Goodpaster, Ph.D. and Lauren M. Sparks, Ph.D. 2017 Metabolic flexibility in health and disease Bret H. Goodpaster, Ph.D. and Lauren M. Sparks, Ph.D. Cell Metab 25(5): 1027–1036
(2) Corey A. Rynders, Stephane Blanc, Nathan DeJong, Daniel H. Bessesen and Audrey Bergouignan. 2018 Sedentary behaviour is a key determinant of metabolic inflexibility. J Physiol 596.8 pp 1319–1330
(3) David E. Kelley. 2005 Skeletal muscle fat oxidation: timing and flexibility are everything. J. Clin. Invest. 115:1699–1702
(4) Jönsson, T., Olsson, S., Ahrén, B. et al. Agrarian diet and diseases of affluence – Do evolutionary novel dietary lectins cause leptin resistance?. BMC Endocr Disord 5, 10 (2005). https://doi.org/10.1186/1472-6823-5-10
(5) De Luca C, Olefsky JM. Inflammation and insulin resistance. FEBS Lett. 2008;582(1):97-105. doi:10.1016/j.febslet.2007.11.057